The 10 Best Probiotics for Women - a Nutritionist's Top Picks
Probiotics are bacteria which offer health benefits to their host. Research shows that different strains of probiotics (types) do different things - they are not 'one-size-fits-all'. Therefore, the best probiotic for women depends on their individual needs. Learn more about probiotics by reading What are probiotics? Of course, many probiotics are beneficial for both women and men, but several strains have been shown to be particularly beneficial in supporting women's gut and intimate health. Read on to find out which are the best women's probiotics.
In this article, we look at:
- How can probiotics help women?
- Vaginal health - best probiotics for women
- Digestive health - best probiotics for women
- Which is the best probiotic for women?
- Should women take probiotics every day?
If you’re short for time, jump to the key take-aways:

How can probiotics help women?
Probiotics are live micro-organisms which offer health benefits to their host. The importance of supporting gut health with probiotics is becoming more widely recognised, but we don't just have a microbiome in our gut, we have them, all over the body, including our mouth, on the skin, in the lungs, and in the vagina. Therefore probiotics are not just used to support a healthy gut, they can be used to support overall health and wellbeing, and a variety of different health concerns, such as:
- Gut health
- Bloating
- Vaginal health
- Skin health
- Immune support
- Pre and post-natal health
- Cholesterol management
- Mood and wellbeing
Follow the links to read in-depth articles on the Probiotics Learning Lab about these various aspects of health, or read on to explore in more detail which probiotics are best for women. Find out which strains are for vaginal health in the next section, or learn about the best probiotics for common female health conditions such as bloating or occasional constipation.
Best probiotics for women's vaginal health
You may ask, what are vaginal probiotics? How are probiotics good for vaginal health? What is the best women’s probiotic for BV and/or thrush? To answer these questions, we first need to think about the anatomy of the intimate area, and how the vaginal microbiome may become unbalanced.
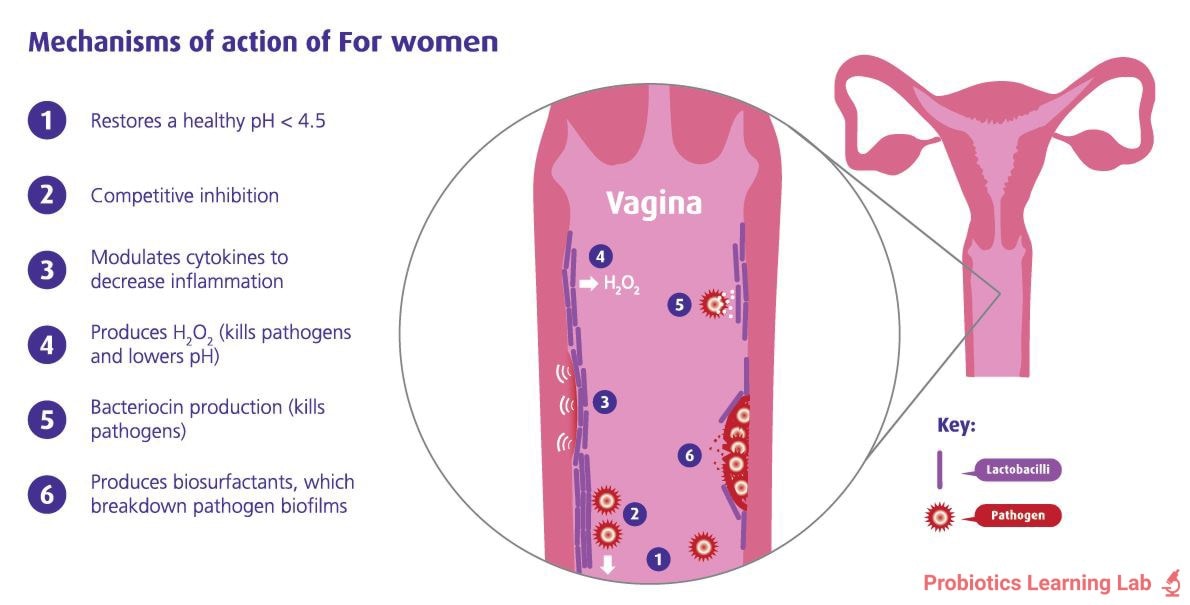
Typically, a healthy vaginal and urinary microbiome will be populated largely by Lactobacilli bacteria. These helpful microbes are thought to exert many of the same beneficial effects as they would in the gut: helping to maintain a healthy balance and discouraging bad bacteria or yeasts from overgrowing and causing conditions such as thrush, urinary tract infections (UTIs) and bacterial vaginosis (BV)1,4. However, due to the proximity of the vagina to the anus,it is much easier for bad bacteria and yeasts to translocate from the gut to the vagina to cause infections that it is for gut bacteria to cause health issues in the penis5.
It is believed that most infections like thrush, cystitis or UTIs stem from bad gut bacteria which have travelled through the digestive tract to the anus, across the perineum and over to the urogenital tract. Thankfully, good bacteria can take the same route! Not all probiotic strains will travel to the vagina, however, so if you are choosing a supplement, make sure it contains specific probiotics for vaginal health. Certain strains such as Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14® have been shown to reach the vagina alive and colonise there, positively affecting the environment. Strains with these abilities are the best vaginal probiotics.
Another common question is "Can you put probiotics into your vagina?" The simple answer to this is "Yes", it's not unsafe to do so; however, probiotics were taken orally in most supporting research studies, so with an oral probiotic supplement containing strains proven to reach the vagina alive, you don't need to. According to the scientists who conducted one study, "L. rhamnosus GR-1® and L. reuteri RC-14® can translocate to the vaginal environment even if they are taken orally" and "Their administration results in significant changes in the vaginal flora in terms of increased Lactobacilli presence…"6.
This means that there is no need to put these probiotics directly into the vagina, and they can be taken easily and more conveniently by mouth.
Healthcare professionals can learn more about the research behind Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14® on the Probiotics Database.
Read on to find out more about the best probiotics for vaginal health and common vaginal infections.
Bacterial vaginosis
As BV is the most common type of vaginal infection in premenopausal women7, finding a safe and natural approach to treatment/prevention would be a huge ‘win’. One significant study, a randomised, placebo-controlled trial8, showed that the vaginal microflora in women with bacterial vaginosis (BV) was restored to a more favourable, Lactobacilli-dominant environment following two months of taking the probiotics Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14®.
During pregnancy, many often suffer from intimate health infections due to the hormonal changes taking place during this time. It is important for both the health of mother and baby that an expectant mother has a healthy vaginal microbiome, as during a normal vaginal delivery the mother passes on some of her resident microflora to her newborn. This transference of bacteria from mother to baby influences the health of the baby’s microbiome.
In 2018 a clinical trial9 showed that the probiotic strain Lactobacillus rhamnosus HN001 (in conjunction with Lactobacillus acidophilus La-14® and lactoferrin) can help reduce symptoms of BV such as itching and discharge.
A clinical trial using Lactobacillus paracasei F-19® demonstrated the ability to improve vaginal pH and odour in those with vaginosis10, maintaining relief even 3 months after the end of treatment when taken orally.
A probiotic designed to supprt BV might contain these strains, as they are some of the most well-researched for this condition.
Anyone with a vagina can develop BV, even those undergoing masculinising hormone therapy11, so it's important to always keep an eye on your vaginal health.
Urinary tract infections
Urinary tract infections (UTIs) unfortunately affect people of all ages. It seems that in the genitourinary area of those who do not experience infections, Lactobacilli bacteria dominate1. The probiotic strains; Lactobacillus rhamnosus GR-1®, Lactobacillus reuteri RC-14®12,27 and Lactobacillus crispatus13 have been reported to support a healthy urinary microbiome in those who experience recurrent UTIs.
Healthcare professionals can learn more around this subject by reading the following articles on the Probiotic Professionals site:
Probiotics for UTIs - a look at the research
Could probiotics help cystitis?
Thrush
Thrush is a very common vaginal complaint. It can occur due to vaginal imbalances caused by hormonal fluctuations at certain points in the menstrual cycle, during pregnancy and when taking the combined oral contraceptive pill or hormonal replacement therapy. When oestrogen levels are high, Candida, the yeast responsible for thrush, thrives14. A probiotic supplement that contains the well-researched Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14® strains may help those prone to thrush, as they may help inhibit the growth of harmful bacteria and yeasts, such as Candida, in the vagina15. It can also occur when the vaginal microbiome is disrupted due to taking antibiotic medications - read more about taking antibiotics and how probiotics can be helpful.
A 2015 study16 looked at 40 women with recurrent vulvovaginal candidiasis (thrush), some were given the probiotic strains Lactobacillus rhamnosus DSM 14870 and Lactobacillus gasseri DSM 14869 alongside conventional treatment. The results showed that probiotics taken alongside conventional treatment increased the efficacy and reduced the risk of the infection coming back compared to conventional treatment alone.
Healthcare professionals can learn more by reading Which probiotics help with thrush? and Which Probiotics are best for Candida? on the Probiotic Professionals site.
Fertility
Vaginal infections including BV, UTIs and Group B Streptococcus (GBS) have been linked to complications in pregnancy and even reducing the chance of getting pregnant in the first place17. It can be an important consideration for any pre-conceptual regime to incorporate a probiotic that addresses the vaginal microbiome, especially if the infections are reoccurring.
The beauty of these specific probiotics is that not only do they reduce symptoms, but they also appear to act against recurrence. For the 1 in 3 people with vaginas who suffer from BV, 30% who suffer recurring cystitis and 75% who suffer thrush at least once, these strains of probiotics could be a welcome addition to their tool kit to rid themselves of these uncomfortable conditions.
Can probiotics make your vagina smell better?
A few years back there was some buzz around a probiotic supplement that claimed to get your vagina smelling like a peach! However, this turned out to be misleading and was not intended to change the smell of the vagina; as far as we know there aren’t any probiotics that can produce a fruity aroma in the vagina!
However, it’s true that when you have a vaginal infection, the smell (e.g. in the case of bacterial vaginosis) can be unpleasant and upsetting. Probiotics can indeed help to solve this problem and get you smelling fresh, naturally!25
Best probiotics for women's digestive health
The vaginal flora is supported by different probiotic strains to those recommended for gut health. Whilst probiotic strains for digestive health conditions are not typically gender-specific, there are a few digestive symptoms which are commonly experienced by women. Women tend to have a slightly longer colon than men, meaning that stool transit time can be longer and women are more likely than men to suffer from IBS-type symptoms such as constipation and bloating2. Other factors, such as pregnancy, menstruation, and other hormonal influences along with differences in lifestyle can also lead to a higher incidence of digestive issues in women3. Let's explore which probiotic strains have been researched for these conditions.
Bloating
Bloating is an extremely common concern. This may be a constant problem, or the bloating may be cyclical and worsen at certain times of the menstrual cycle (e.g. premenstrual bloating) or around menopause.
Healthcare professionals can learn more by reading Could probiotics help with menopause symptoms? on the Probiotic Professionals site.
There are several factors that can lead to a swollen, uncomfortable abdomen: fluctuating hormone levels, stress, poor diet or disturbed digestion (IBS, food intolerances for example), to name a few. Upset digestion associated with menstruation is very common, including alterations to bowel patterns, constipation, diarrhoea, nausea, abdominal pain and bloating18. Fluctuating levels of female sex hormones, oestrogen and progesterone, and the body’s sensitivity to these fluctuations is thought to contribute to the sensation of bloating that occurs around menstruation19. Certain probiotic strains may help to alleviate this occasional bloating and digestive discomfort, such as Lactobacillus acidophilus NCFM®.
Additionally, Bacillus coagulans Unique IS-2 was shown in a gold-standard clinical trial to reduce symptoms of IBS in adults20. From week five the probiotic group exhibited significant improvements in abdominal discomfort, occasional bloating, urgency, incomplete evacuation, straining, passage of gas and bowel habit satisfaction.
Bacillus coagulans Unique IS-2 is part of a group of bacteria known as soil-based organisms which are commonly used in food, beverage and gummy supplement production due to the robust nature of this bacteria.
Health professionals can read more about Lactobacillus acidophilus NCFM® and Bacillus coagulans Unique IS-2 on the Probiotics Database.
You may like to read the following blog: Bloating – all you need to know to learn more.

Many women experience a bloated stomach in menopause that might be relieved with a few simple measures to look after their gut health, and the health of the microbiome. However, persistent bloating should never be overlooked and should be investigated by a GP, as bloating can be signs of more serious conditions.
Occasional Constipation
As previously mentioned, constipation is more frequently reported in (cisgender) women than men21, often occurring around menstruation, during pregnancy and post-menopause. A probiotic supplement containing Bifidobacterium lactis BB-12® can help support gut health in those with occasional constipation. B. lactis BB-12®, along with fructooligosaccharides (a prebiotic), can help gently encourage regular bowel movements, as supported by one of the largest clinical trials performed on probiotics22. This probiotic is often used by women with regularity issues.
Health professionals can read more about the research behind this strain on the Probiotics Database: Bifidobacterium lactis BB-12®.
Alterations to normal bowel patterns, including occasional constipation, can also occur as a part of irritable bowel syndrome (IBS). Symptoms of IBS, including abdominal discomfort and disrupted bowel patterns, can be exacerbated around the time of menstruation in those with menstrual cycles and in perimenopausal women23.
To learn more about how to support gut health in IBS, read Which probiotics are for IBS?
For more information about supporting clients with occasional constipation, healthcare professionals can read Probiotics for Constipation on the Probiotic Professionals site.
Pregnancy
Some strains of probiotics such as Lactobacillus rhamnosus HN001, Lactobacillus acidophilus La-14®, and Bifidobacterium lactis HN019, have been researched specifically in pregnancy and found to support common pregnancy-related concerns such as digestive issues, morning sickness, gestational diabetes, and mental wellbeing.
For everything you need to know about using probiotics at this special time, read Probiotics for Pregnancy.
Which is the best probiotic for women?
It can be confusing to know how to choose the best probiotic for women, as there are many different types of probiotic supplements available, including capsules, liquids and powders, but most women tend to prefer a capsule as these are easy to fit into a morning routine. For women who really don’t like capsules or powders, then gummy products for adults are now available. However, it is important to select gummies which contain very robust strains of bacteria (known as soil-based organisms) which allows them to survive the manufacturing process, for example Bacillus coagulans Unique IS-2.
It's good to look for the most recommended probiotics, so check out the reviews for your chosen brand. But the most effective probiotic for women will be the one which is most suitable for their individual needs. Therefore if you are seeking specific health benefits, such as the best probiotic for women over 50, consider a friendly bacteria supplement with research supporting its use for this particular purpose. For example, if you are looking for probiotics for vaginal health, consider a product that contains well-researched strains including L. paracasei F-19® and the world-renowned L. rhamnosus GR-1® and L. reuteri RC-14® which have shown to help support a healthy vaginal microbiome24.
If you’re confused as to what ‘well-researched’ really means, what is meant by terms such as 'billions CFU', or why research is so important, Dr. Kate explains all in this helpful article: Research: is it all equal?.
If you’ve never taken probiotics before and are wondering if they’d suit you, then be reassured that the potential benefits of probiotics are numerous, but any side effects are rare, making these supplements a popular choice for daily maintenance of gut and intimate health.
Healthcare professionals can reassure their clients about this topic by reading Probiotics and side effects – an in-depth review on the Probiotic Professionals site.
Should women take probiotics every day?
With a very few exceptions, it is safe - and often advisable - for women to take probiotics every day. Read more about using probiotics daily in this in-depth article: Can I take probiotics every day? If you have serious health conditions or are taking medication, then speak to your doctor before taking any natural supplement.
Key Take-aways
- Probiotic supplements are not usually gender-specific, but certain strains have been researched specifically for the support of female health issues such as vaginal infections, and pregnancy.
- Probiotics can help to limit the overgrowth of harmful bacteria and yeasts that contribute to the development of gut and intimate health issues.
- Women often suffer from digestive issues, such as occasional constipation and bloating, more often than men.
- The vagina and urinary tract require different friendly bacteria to the gut to maintain a healthy microbiome.
- Look for specific probiotic strains which have been researched for your individual needs.
The 10 Best Rated Probiotics for Women
- Lactobacillus rhamnosus GR-1® - vaginal health
- Lactobacillus reuteri RC-14® - vaginal health
- Lactobacillus paracasei F-19® - vaginal health
- Lactobacillus rhamnosus HN001 - vaginal health
- Lactobacillus crispatus - vaginal health
- Lactobacillus acidophilus NCFM® - bloating and IBS
- Bifidobacterium lactis BB-12® - occasional constipation and regularity
- Bacillus coagulans Unique IS-2 - IBS
- Lactobacillus rhamnosus HN001 - pregnancy
- Bifidobacterium lactis HN019 - pregnancy
For more information about other supplements for women’s health, read Kathy’s article: Supplements for women: which do you really need?.
You may also be interested to read the following related articles:
References
- Komesu YM et al. Defining the relationship between vaginal and urinary microbiomes. Am J Obstet Gynecol. 2020;222(2). doi:10.1016/j.ajog.2019.08.011.DEFINING
- Kim YS, Kim N. Sex-Gender Differences in Irritable Bowel Syndrome. J Neurogastroenterol Motil 2018;24:544-558. https://doi.org/10.5056/jnm18082
- Utano, K., Nagata, K., Honda, T. et al. Bowel habits and gender correlate with colon length measured by CT colonography. Jpn J Radiol 40, 298–307 (2022). https://doi.org/10.1007/s11604-021-01204-7
- Witkin SS, Linhares IM. Why do lactobacilli dominate the human vaginal microbiota? BJOG An Int J Obstet Gynaecol. 2017;124(4):606-611. doi:10.1111/1471-0528.14390
- Magruder M, Sholi AN, Gong C, et al. Gut uropathogen abundance is a risk factor for development of bacteriuria and urinary tract infection. Nat Commun. 2019;10(1). doi:10.1038/s41467-019-13467-w
- Morelli L, Zonenenschain D, Del Piano M, Cognein P. Utilization of the intestinal tract as a delivery system for urogenital probiotics. J Clin Gastroenterol. 2004;38(6 Suppl). doi:10.1097/01.mcg.0000128938.32835.98
- BASHH. Sexually Transmitted Infections in Primary Care 2013. 2014. https://www.bashhguidelines.org/media/1089/sexually-transmitted-infections-in-primary-care-2013.pdf.
- Reid G, Burton J, Hammond JA, Bruce AW. Nucleic acid-based diagnosis of bacterial vaginosis and improved management using probiotic lactobacilli. J Med Food. 2004;7(2):223-228. doi:10.1089/1096620041224166
- Russo R, Karadja E, De Seta F. Evidence-based mixture containing Lactobacillus strains and lactoferrin to prevent recurrent bacterial vaginosis: A double blind, placebo controlled, randomised clinical trial. Benef Microbes. 2019;10(1):19-26. doi:10.3920/BM2018.0075
- A. Delia, G. Mordante, G. Rago, M. C. Musaccmio, K Retaglia, V De Leo. (2006). Efficacia dell'utilizzo dtìLactobacillus paracasei subsp. paracasei F19 nella vaginosi e nella prevenzione delle recidive di vaginite somministrato per via orale contemporaneamente ad un Lactobacillus acidofilusptr via vaginale. Minkrva Ginkcoi. 2 (56), 227-3.
- Land, E., 2021. Q&A: Gynecologic and vaginal care for trans men - San Francisco AIDS Foundation. [online] San Francisco AIDS Foundation. Available at: <https://www.sfaf.org/collections/beta/qa-gynecologic-and-vaginal-care-for-trans-men/> [Accessed 17 August 2021].
- Beerepoot MAJ, Mostert). Women with Recurrent Urinary Tract Infections : Antibiotic Resistance and Non-Antibiotic Prophylaxis. [s.n.]; 2013. https://dare.uva.nl/search?identifier=381af002-2eb8-4956-834f-3aef23760310. Accessed February 15, 2018.
- Stapleton AE, Au-Yeung M, Hooton TM, et al. Randomized, placebo-controlled phase 2 trial of a lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis. 2011;52(10):1212-1217. doi:10.1093/cid/cir183
- Dennerstein GJ, Ellis DH. Oestrogen, glycogen and vaginal candidiasis. Aust New Zeal J Obstet Gynaecol. 2001;41(3):326-328. doi:10.1111/j.1479-828X.2001.tb01238.x
- Martinez RCR, Franceschini SA, Patta MC, et al. Improved treatment of vulvovaginal candidiasis with f********** plus probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. Lett Appl Microbiol. 2009;48(3):269-274. doi:10.1111/j.1472-765X.2008.02477.x
- Sonal Pendharkar, Erik Brandsborg, Lennart Hammarström, Harold Marcotte & Per-Göran Larsson. (2015). Vaginal colonisation by probiotic lactobacilli and clinical outcome in women conventionally treated for bacterial vaginosis and yeast infection. BMC Infectious Diseases. 255 (6), 0971-3.
- Michael D Harwich Jr, Joao M Alves, Gregory A Buck, Jerome F Strauss III, Jennifer L Patterson, Aminat T Oki, Philippe H Girerd & Kimberly K Jefferson. (2010). Drawing the line between commensal and pathogenic Gardnerella vaginalis through genome analysis and virulence studies. BMC Genomics volume. 11 (4), 375.
- Bernstein MT, Graff LA, Avery L, Palatnick C, Parnerowski K, Targownik LE. Gastrointestinal symptoms before and during menses in healthy women. BMC Womens Health. 2014;14(1). doi:10.1186/1472-6874-14-14
- Yonkers KA, O’Brien PS, Eriksson E. Premenstrual syndrome. Lancet. 2008;371(9619):1200-1210. doi:10.1016/S0140-6736(08)60527-9
- Madempudi, R. S. et al. (2019) ‘Randomized clinical trial: the effect of probiotic Bacillus coagulans Unique IS2 vs. placebo on the symptoms management of irritable bowel syndrome in adults’, Scientific Reports, 9(1). doi: 10.1038/s41598-019-48554-x.
- Verkuijl SJ, Meinds RJ, Trzpis M, Broens PMA. The influence of demographic characteristics on constipation symptoms: A detailed overview. BMC Gastroenterol. 2020;20(1):1-9. doi:10.1186/s12876-020-01306-y
- Eskesen D, Jespersen L, Michelsen B, Whorwell PJ, Müller-Lissner S, Morberg CM. Effect of the probiotic strain Bifidobacterium animalis subsp. lactis, BB-12®, on defecation frequency in healthy subjects with low defecation frequency and abdominal discomfort: A randomised, double-blind, placebo-controlled, parallel-group trial. Br J Nutr. 2015;114(10):1638-1646. doi:10.1017/S0007114515003347
- Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend Med. 2009;6(PART 2):152-167. doi:10.1016/j.genm.2009.03.004
- Reid G, Beuerman D, Heinemann C, Bruce AW. Probiotic Lactobacillus dose required to restore and maintain a normal vaginal flora. FEMS Immunol Med Microbiol. 2001;32(1):37-41. doi:10.1016/S0928-8244(01)00269-3
- Kellogg Spadt S, et al. Abstract P-35. Presented at: North American Menopause Society Annual Meeting; Oct. 12-15, 2022; Atlanta.
- Moreno, I. et al., (2022) Endometrial microbiota composition is associated with reproductive outcome in infertile patients. Microbiome, 10:1 https://doi.org/10.1186/s40168-021-01184-w
- New, F.J. et al., (2022) Role of Probiotics for Recurrent UTIs in the Twenty-First Century: a Systematic Review of Literature. Curr Urol Rep 23, 19–28 (2022). https://doi.org/10.1007/s11934-022-01085-x
Popular Articles
View all Women's Health articles-
General Health08 Mar 2024
-
General Health06 Dec 2023
-
General Health04 Mar 2024



