The Best Probiotics for IBS, According to a Nutritionist
Could probiotics help your IBS symptoms? Read on to find out how probiotics are good for IBS; how to choose the best probiotics for IBS and what to look for in a probiotic supplement for IBS. Or if you're in a hurry, watch my short IBS information video in which I explain how to choose the best probiotics for IBS and your IBS type.
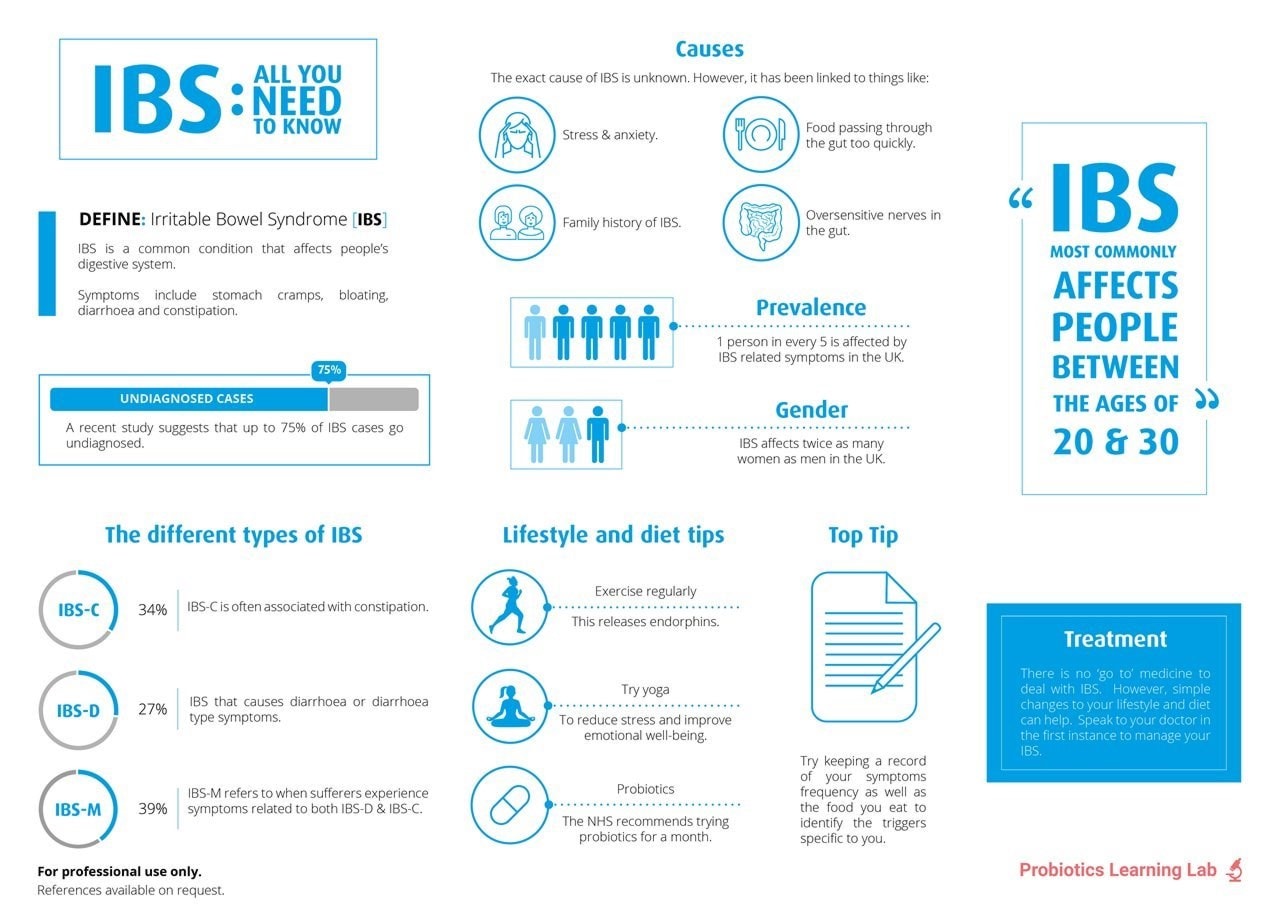
Irritable bowel syndrome, known as IBS, is an increasingly common disorder of the digestive system affecting up to 20% of the UK population, with women twice as likely to be affected as men. There is no known medical cure or specific cause, and every individual's symptoms can be different, so IBS treatment typically focuses on symptom management. However, symptoms may be exacerbated by foods such as wheat and dairy products, high FODMAP foods, and lifestyle factors such as stress, or an imbalance of good bacteria and bad bacteria in the gut5.
Therefore many people find that diet and lifestyle improvements can provide IBS relief, and it can be a good idea to keep a food and symptom diary for a few weeks to see if certain foods trigger your symptoms. Natural supplements are also very popular, with probiotics for IBS becoming a go-to supplement for many sufferers.
Which probiotics are best for IBS?
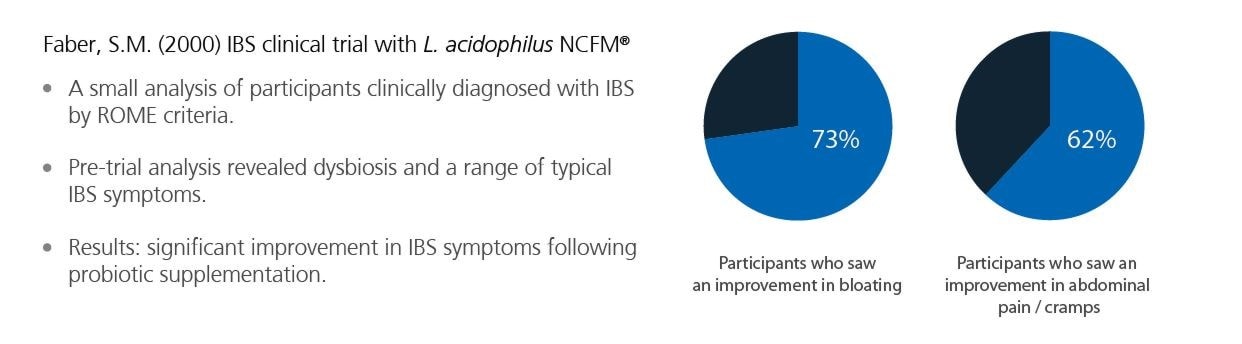
IBS has a broad range of symptoms, and you should look for supplements containing well-researched probiotic strains which have been found to offer benefits for your particular symptoms. It can also be worthwhile taking a high-quality daily product for all-round gut support alongside your specific strains. My personal favourite 'all-rounder' strain for IBS is Lactobacillus acidophilus NCFM® which has been shown to help with a variety of typical IBS symptoms::
- Abdominal discomfort
- Gas/Bloating
- Poor gut motility
- Loose stools
- Bowel regularity
Research15,29 shows this strain is a great all-rounder and would be helpful to support all types of IBS, so ideally your daily product would have this strain in it. But a review of all available research to date confirms that specific probiotics have a beneficial role to play in chronic disorders like IBS28, and people often take an all-round product for general gut support alongside one containing strains to support their specific type of IBS, such as the following:
- For IBS-D & post-infectious IBS - Saccharomyces boulardii
- For IBS-C - Bifidobacterium lactis BB-12®
Please note: if you are experiencing severe IBS symptoms, you must always speak to your doctor for advice.
So probiotics and IBS are currently a huge area of interest, but how do you know which probiotics are good for IBS symptoms, or which type of IBS you have? There are different types of IBS, and the most used method for diagnosing IBS is the Rome criteria, which classifies IBS into these different categories - click on the one which suits your symptoms best, or watch my short video below:
- IBS-D – Diarrhea predominant
- IBS-C – Constipation predominant
- IBS-A – Alternating constipation & diarrhea
- IBS-U – Unspecified & varying symptoms
- Post-infectious IBS
If you have a general question about IBS, check out our information sections below:
- Do probiotics help IBS?
- Can probiotics make IBS worse?
- IBS and bloating
- Prebiotics for IBS
- NHS recommends probiotics for IBS
- Which probiotics are best for IBS
Do probiotics help IBS?
We're often asked questions about probiotics and IBS, such as "Can you treat IBS with probiotics?", "Should IBS sufferers take probiotics?", and simply "Are probiotics good for IBS?"! The answer is that probiotics have been shown in many clinical trials to help the symptoms of IBS, and most sufferers find them useful. Even the NHS recommends probiotics for IBS - they are fine to take alongside most prescription and over the counter medications for IBS, and are a safe, natural option to try. However, if you think you have IBS, you should always have your symptoms diagnosed by a doctor first.
But how do probiotics help IBS? Probiotics may help IBS because the condition has been associated with an imbalance in the gut microbiome5, the name for the populations of live bacteria that live in the gut. Read more about the gut microbiome in this article: All About the Microbiome.
Recent research seems to confirm this, indicating a link between IBS-D symptoms and a harmful bacteria called Brachyspira22. IBS sufferers often have lower levels of good bacteria e.g. Bifidobacterium species, and increased levels of bad bacteria, known as pathogens, with some of the best-known being from the Clostridium species. Supplementing with a high-quality probiotic may help to reduce IBS symptoms in the following ways:
- Probiotic bacteria give a huge boost to the number of friendly bacteria in the gut, leaving less space for ‘bad’ microbes that may cause IBS symptoms.
- Beneficial bacteria help break down problem foods that may exacerbate IBS.
- A healthy gut microbiome may play a part in reducing the impact of stress on the gut, which is a key factor for many people with IBS.
Read more about the gut-brain connection in this article: The Gut-Brain Axis
When choosing a probiotic supplement for IBS, it is important to select one which is supported by good quality research. It should contain probiotic strains (also known as 'friendly bacteria' or 'live cultures') which have been ‘scientifically tested’ in clinical trials rather than just laboratory studies. Clinical trials show how the probiotic performs in real people, for typical symptoms of IBS, such as constipation, bloating, or diarrhoea. Different probiotic strains can be beneficial for different symptoms of IBS, as each strain can have unique properties.
Clinical studies show the best probiotic supplements for IBS contain strains such as:
- Saccharomyces boulardii
- Bifidobacterium lactis BB-12®
- Lactobacillus acidophilus NCFM®
- Bifidobacterium lactis Bi-07®
- Bifidobacterium infantis 35624
- Bacillus coagulans Unique IS-2
- Bifidobacterium lactis HN019
- Lactobacillus plantarum Lp299v®
Read on to find out more about these strains, or if you're short on time, why not watch the video below watch my short IBS information video.
I give a brief overview of the best strains to use for the most common types of IBS
Can probiotics make IBS worse?
Probiotics are natural and well tolerated by the majority of people who take them. Those who have an extreme imbalance of good and bad bacteria in their gut, also known as dysbiosis, may notice some changes in their digestive system when they first start to take a probiotic supplement. These side effects should subside within 48 hours in most people while the gut microbiome readjusts, but may last a little longer if the gut is severely imbalanced. If you can, it is worth persevering, either by lowering the dose or coming off for a few days before reintroducing them, once the gut has readjusted the pre and probiotics can start to exert their full benefits. Probiotic supplements which contain prebiotics may also cause an increase in gas and bloating, especially in those who are sensitive to certain carbohydrates. For those who are on a low FODMAP diet, prebiotic or synbiotic supplementation is generally avoided at this time.
Read more about FODMAPs and prebiotics in What are Prebiotics?
Healthcare professionals may wish to read more about this over on our Probiotic Professionals site: Probiotics and Side Effects - an in-depth review.
Probiotics for IBS-D
If your doctor diagnoses you with IBS and your primary symptom is diarrhea, then you have IBS-D. Saccharomyces boulardii is one of the best probiotics for IBS-D symptoms.
This unique probiotic is in fact a yeast, the only yeast 'friendly' enough to be called a probiotic.S. boulardii has over 50 years of research supporting its use, and is recommended in many hospitals worldwide for diarrhoea. You can find this strain in Optibac Probiotics S. boulardii.
A 2021 review of 42 clinical trials confirmed S. boulardii as one of the best probiotic strains for IBS diarrhoea27. The review showed that S. boulardii offered significant improvements in abdominal pain and frequency of bowel movements for individuals with IBS-D. As well as IBS-D, S. boulardii has also been shown to be beneficial for oocasional diarrhoea associated with Inflammatory Bowel Disease (IBD), antibiotic-associated diarrhoea and traveller’s diarrhoea. Healthcare practitioners can read more about probiotics for IBD on the Probiotic Professionals site.
As S. boulardii is a friendly yeast, it has very different properties to friendly bacteria: it's a 'transient' probiotic which means it does not colonise for long in the gut. Therefore it’s a good idea to take a probiotic containing colonising friendly bacteria alongside S. boulardii as they work together. For this, use one of the probiotic strain recommendations in the IBS-A section.
The probiotic strains Pediococcus acidilactici CECT 7483, Lactobacillus plantarum CECT 7484 and Lactobacillus plantarum CECT 7485 have also been researched and shown to be good probiotics for IBS-D13. This trial measured improvements in the quality of life of the participants, in relation to their IBS diarrhoea symptoms, which is thought to be one of the most accurate ways of measuring the effectiveness of the treatment.
However, Saccharomyces boulardii is the primary probiotic recommendation for IBS-D. Healthcare practitioners can read more about S. boulardii and using probiotics for diarrhoea and upset stomachs on the Probiotics Professionals site.

Probiotics for IBS-C
If you have IBS which presents with regularity issues and constipation, this is known as IBS-C. There are a couple of strains which have been particularly researched for constipation: Bifidobacterium lactis BB-12® and Bifidobacterium lactis HN019. Bifidobacteria like to live in the large intestine where the stool is formed, so they tend to be the most researched probiotic for regularity issues.
Bifidobacterium lactis BB-12® , is thought to be the most well-researched strain in the whole Bifidobacteria family, and has been particularly researched in those with constipation3,4. It promotes more regular bowel movements, which are easier to pass, as well as supporting gut health in general.
In one clinical trial, over 100 women with a tendency towards constipation were given a supplement containing Bifidobacterium lactis BB-12® and prebiotics14. Intestinal transit time (the time it takes for food to move through the gut) decreased significantly. Those who took the B. lactis BB-12® supplement were no longer constipated and had normal bowel movements compared to those who took the placebo.
The above illustrated clinical trial used Bifidobacterium lactis BB-12® in combination with a prebiotic; however, prebiotics don't suit everyone who suffers from IBS. Read more about prebiotics and IBS below.
The probiotic strain Bifidobacterium lactis HN019 has been researched for all symptoms of IBS, and more specifically to improve intestinal transit time10. IBS-C sufferers who prefer to avoid prebiotics may get on better with a supplement containing Bifidobacterium lactis HN019 without added prebiotics. Healthcare professionals can learn more about Bifidobacterium lactis HN019 on the Probiotics Database.
Healthcare professionals can learn more about using probiotics for constipation on the Probiotic Professionals site, and read the rest of the research involving Bifidobacterium lactis BB-12® and Bifidobacterium lactis HN019 on the Probiotics Database.
Probiotics for IBS-A (also known as IBS-M)
Many people with this type of the condition find they have alternating symptoms of IBS diarrhoea, bloating, pain, and constipation. This form of IBS is known as IBS-A (alternating) or IBS-M (mixed symptoms). For the relief of this IBS variant, it can be hard to know which symptom to target, but the best first step is to try a high-quality, general, daily probiotic for all-round gut-support, as imbalanced gut flora is thought to be a factor in IBS5. Two strains, Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07® which can be found in Optibac Probiotics Every Day EXTRA have been specifically trialled in those with IBS and found to not only regulate bowel movements29 but also for the relief of IBS bloating, abdominal distension, and abdominal cramps15.
Even on its own Lactobacillus acidophilus NCFM® has been shown to be effective in improving various symptoms of patients with IBS5,6.
Healthcare professionals can read more about Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07® on the Probiotics Database.
Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07® are the most recommended strains for all-round IBS support, but there a few other probiotic strains which can be considered:
The probiotic strain Bacillus coagulans Unique IS-2, is often used in 'gummy' probiotic supplements so is popular with people who find this format easier to take. It can be found in Optibac Probiotics Gut Health Gummies, and has been researched for the support of IBS symptoms in both adults and children. In one study involving 136 adults with IBS were given eight weeks. A significant reduction in abdominal pain and an increase in the number of normal bowel movements was noted, compared with the placebo group26.
Healthcare professionals can visit B. coagulans Unique IS-2 to find out more about the research using this strain.
Bifidobacterium infantis 35624 , also known as 'Bifantis’, has been researched in those with Irritable Bowel Syndrome with positive results8. An 8-week trial with 75 participants associated B. infantis 35624 with a reduction in pain, discomfort, bloating and constipation. Healthcare practitioners can refer to Bifidobacterium infantis 35624, which has more information on this strain.
A specific strain of the Lactobacillus plantarum species (L. plantarum Lp299v®) has also been clinically trialled on participants with IBS diarrhoea, bloating, and constipation and shown to reduce IBS symptoms16. A 4-week clinical trial of 60 IBS sufferers showed that those in the probiotic group had a decrease in flatulence and pain and more consistent bowel movements. Healthcare practitioners can visit this page on the Probiotics Database L. plantarum Lp299v® to find out more related research.
Probiotics for IBS-U
If the previous types of IBS do not sound quite like you, then you might be struggling with IBS-U (Undefined or Unclassified). This form of IBS is characterised by a stool consistency that doesn't fit into the other categories.Sufferers may experience both loose, watery stools and harder stools, but both less than 25% of the time. This IBS type tends to be less common than the others but has similar causes, including diet or an imbalance of bacteria in the gut and bowels. There is also evidence to suggest a gut-brain connection17.
Again, as with IBS-A/M above, it's best to begin supporting this type of IBS with probiotic strains which have been shown to help with a variety of symptoms, such as Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07®. After supplementing with these strains for a month or so, symptoms may improve fully, or begin to trend more towards one symptom, then it will be possible to add in more specific strains for more targeted support. It's also wise to consider triggers so keeping an IBS symptom diary can be helpful.
Post-infectious IBS
Approximately one in ten people who suffer from IBS believe their symptoms began with an upset stomach. Serious infections such as gastroenteritis or parasitic infections are more likely to cause this sort of IBS18. It seems that there are a couple of risk factors for developing post-infectious IBS, including the duration of the illness, whether you are a smoker, female, suffer from depression, or experienced any adverse life events three months previously19.
If you have this type of IBS, you are more likely to suffer from diarrhea or a mixed stool pattern. Taking the probiotic yeast Saccharomyces boulardii can help address the cause of the infectious illness30 itself and also support the IBS symptoms afterwards. It may also be prudent to take a general probiotic alongside to assist with other associated symptoms.
IBS and bloating
People with all forms of IBS may also suffer from occasional bloating. It can be aggravated by factors such as stress or eating particular foods which challenge the digestive system23, for example, gluten- or dairy-containing foods. However, as mentioned, many different high-quality probiotic strains have been shown to alleviate and prevent pain and IBS bloating, including Lactobacillus acidophilus NCFM®, Bifidobacterium lactis Bi-07® 15 and Bifidobacterium infantis 356248. Strains like Lactococcus casei Rosell-1058 assist with the digestion of problem foods by producing enzymes which break down starch and lactose. Learn more by reading: Probiotics for bloating.
At the end of the day, everyone is different, and IBS bloating sufferers will have different gut floras to one another. With probiotics, it is often a case of trial and error to find which species and strains work for that individual. There is no harm, in 'mixing and matching' different products if this works for you. You can't take 'too many' probiotics. For more information on this topic, see Is it possible to overdose on probiotics?

Prebiotics for IBS
Due to some prebiotic foods causing adverse reactions in those with IBS, we often get asked "Are prebiotics good for IBS" and if so "Which are the best prebiotics for IBS?".
If you experience bloating or digestive discomfort when eating particular prebiotic foods, you may be wondering whether to choose a prebiotic or probiotic for IBS, or a combination called a synbiotic without irritating your gut.
If you’re highly sensitive to foods that fall into the high FODMAP category, such as garlic, onions, apples, and leeks I firstly recommend working with a professional to try a low FODMAP diet to help calm your gut. During the elimination phase (which should only be a total of 4 weeks) you will be advised to avoid most prebiotic supplements.
For those who are mostly fine with prebiotic foods, what prebiotic supplements for IBS are best? Well, research shows that high dose synbiotic supplements including Fructooligosaccharides (FOS) were superior to placebo in improving bowel symptoms and fatigue in those with IBS20. Prebiotics for IBS-C can be supportive as FOS is a source of soluble fibre that adds bulk and absorbs water to help soften the stool, it also helps encourage peristalsis which is the movement of food through the gut. Prebiotics such as FOS will also stimulate the growth of other beneficial bacteria which is already present in the gut.
Prebiotics for IBS and bloating:
- If you’re worried that introducing prebiotics for IBS will cause bloating, start low and slow! Taking them in the evening before bed can help too.
- Prebiotics are food for your gut bacteria and significantly increase levels of Bifidobacteria in those with IBS21
- When it comes to a probiotic vs prebiotic for IBS, you may need to experiment to see what suits you best.
Learn more about prebiotics, prebiotic foods, and the FODMAP diet by reading: What are prebiotics?
NHS recommends probiotics for IBS
The NHS includes the use of probiotics as part of tips recommended to help relieve IBS symptoms23,31.
This is a big milestone in the world of probiotics because, although probiotics are routinely prescribed in many European hospitals, it wasn’t always part of the NHS recommendations. The NICE guidelines (National Institute for Health and Clinical Excellence), which provides evidence-based guidelines/framework that many medical and health care professionals work within, now recommends that probiotics can be used for at least 4 weeks for managing IBS related symptoms24.
The NHS website states that: "Probiotics may help reduce bloating and flatulence in some people with IBS."
The inclusion of probiotics for IBS relief was due to the result of a systematic review by Moayyedi et al., published in 2010, which concluded that probiotics were effective in the management of IBS25.
If you enjoyed this article, you may also like to read:
Healthcare professionals can find out more by reading the following article on the Probiotic Professionals site:
References
- Das S, et al. (2016) Efficacy and Safety of Saccharomyces boulardii in Acute Rotavirus Diarrhea: Double Blind Randomized Controlled Trial from a Developing Country. J Trop Pediatr. Dec;62(6):464-470
- Wan CM, et al (2017) A multicenter randomized controlled study of Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea in infants and young children. 4;55(5):349-354.
- Eskesen, D. et al. (2015), ‘Effect of the probiotic strain Bifidobacterium animalis subsp. lactis BB-12® on defecation frequency in healthy subjects with low defecation frequency and abnormal discomfort: a randomised, double-blind, placebo-controlled, parallel-group trial’, British Journal of Nutrition, Nov 28: 114(10) :1638–1646.
- Nishida, S. et al. (2004), ‘Effect of Yoghurt Containing Bifidobacterium lactis BB-12® on Improvement of Defecation and Fecal Microflora of Healthy Female Adults’, Milk Science, 53(2):71-80
- Faber, S.M. (2000) 'Treatment of abnormal gut flora symptoms in patients with irritable bowel syndrome'. Am J Gastroenterol 95(9):25333
- Lyra, A. et al., (2016) ‘Irritable bowel syndrome symptom severity improves equally with probiotic and placebo’. World Journal of Gastroenterology. 22 (48):10631–10642.
- O’Mahony L. et al (2005), ‘Lactobacillus and Bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles, Gastroenterology, 128(3):541-51.
- Whorwell PJ et al. (2006) 'Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome.' Am J Gastroenterol 101 7 1581-90.
- Ibarra, A. et al., (2018) ‘Effects of 28-day Bifidobacterium animalis subsp. lactis HN019 supplementation on colonic transit time and gastrointestinal symptoms in adults with functional constipation: A double-blind, randomized, placebo-controlled, and dose-ranging trial’. Gut Microbes, 9(3):236-251.
- Waller, P. A. et al., (2011) ‘Dose-response effect of Bifidobacterium lactis HN019 on whole gut transit time and functional gastrointestinal symptoms in adults’. Scandinavian Journal of Gastroenterology. 1057–1064
- Nobaek S. et al., (2000), ‘Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome’, Am. J. Gastroenterol. 95:1231-1238.
- Ducrotté P. et al., (2012). ‘Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome’. World Journal of Gastroenterology, 18:4012-4018.
- Lorenzo-Zúñiga V et al. (2014) I.31, a new combination of probiotics, improves irritable bowel syndrome-related quality of life. World J Gastroenterol 20 26 8709-16
- Malpeli, A. et al (2012) 'Randomised, double-blind and placebo-controlled study of the effect of a synbiotic dairy product on orocecal transit time in healthy adult women'. Nutr Hosp 27 4 1314-9.
- Ringel-Kulka, T. et al (2011) 'Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: a double-blind study'. J Clin Gastroenterol 45 6 518-25.
- Niedzielin K et al. (2001) 'A controlled, double-blind, randomized study on the efficacy of Lactobacillus plantarum 299V in patients with irritable bowel syndrome'. Eur J Gastroenterol Hepatol 13 10 1143-7.
- Mayer E, A. (2018). The Role of Gut-Brain Interactions in Influencing Symptoms of Irritable Bowel Syndrome. Gastroenterol Hepatol (N Y), 14(1):44–46.
- Lekha Saha. (2014). Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol.. 20 (22), 6759–6773.
- Robin Spiller, Klara Garsed. (2009). Postinfectious Irritable Bowel Syndrome. Gastroenterology. 136 (6), 1979-1988.
- Sang-Hoon Lee , Doo-Yeoun Cho , Seok-Hoon Lee , Kyung-Sun Han , Sung-Won Yan. (2019). A Randomized Clinical Trial of Synbiotics in Irritable Bowel Syndrome: Dose-Dependent Effects on Gastrointestinal Sympto. Korean J Fam Med. 1(40), pp.2-8. [Online]. Available at: 10.4082/kjfm.17.0064 [Accessed 19 May 2023].
- Bridgette Wilson, Megan Rossi, Eirini Dimidi, Kevin Whelan. (2019). Prebiotics in irritable bowel syndrome and other functional bowel disorders in adults: a systematic review and meta-anal. The American Journal of Clinical Nutrition. 109(4), p.1098–1111. [Online]. Available at: https://doi.org/10.1093/ajcn/nqy376 [Accessed 19 May 2023].
- Karolina S Jabbar, Brendan Dolan, Lisbeth Eklunde, Catharina Wising, Anna Ermund, Åsa Johansson, Hans Törnblom, Magnus Simren, Gunnar C Hansson. (2020). Association between Brachyspira and irritable bowel syndrome with diarrhoea. Gut. 0 (0), 1-13.
- NHS, 2017. NHS Choices. [Online] Available at: https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/diet-lifestyle-and-medicines/[Accessed 29 March 2018].
- NICE, 2017. NICE (National Institute for Health and Care Excellence). [Online] Available at: https://www.nice.org.uk/guidance/cg61/chapter/1-Recommendations[Accessed 29 March 2018].
- Moayyedi P, Ford AC, Talley NJ, et al. 2010 The efficacy of probiotics in the treatment of irritable bowel syndrome: a systematic review. Gut. 59(3):325-332. doi:10.1136/gut.2008.167270
- Madempudi, R. S. et al. (2019) ‘Randomized clinical trial: the effect of probiotic Bacillus coagulans Unique IS2 vs. placebo on the symptoms management of irritable bowel syndrome in adults’, Scientific Reports, 9(1). doi: 10.1038/s41598-019-48554-x.
- McFarland L, Karakan T, Karatas A (2021) Strain-specific and outcome-specific efficacy of probiotics for the treatment of irritable bowel syndrome: A systematic review and meta-analysis. eClinicalMedicine, 41: 101154
- Satish Kumar L, Pugalenthi L, Ahmad M, et al. (April 18, 2022) Probiotics in Irritable Bowel Syndrome: A Review of Their Therapeutic Role. Cureus 14(4): e24240. doi:10.7759/cureus.24240
- Magro, D.O., et al., (2014). ‘Effect of yogurt containing polydextrose, Lactobacillus acidophilus NCFM and Bifidobacterium lactis HN019: a randomized, double-blind, controlled study in chronic constipation’. Nutrition Journal, 13:75.
- Kirchhelle A. et al., (1996), ‘Treatment of persistent diarrhoea with Saccharomyces boulardii in returning travellers: results of a prospective study’. Fortschr. Med.114(11):136-140.
- NHS: (2018). Probiotics.[Online] https://www.nhs.uk/conditions/probiotics/ [Accessed 1st September 2022]
- Zhang Jindong,Zheng Haonan,Zhang Tao,Duan Liping, (2022) Effect of Microbiota-targeted Therapy on Gut Microbiota in Patients with Irritable Bowel Syndrome: A Scoping Review. Chinese General Practice.
- Shrestha B et al., (2022) The Role of Gut-Microbiota in the Pathophysiology and Therapy of Irritable Bowel Syndrome: A Systematic Review. Cureus, 14(8): e28064. doi:10.7759/cureus.28064
- Chuah KH. et al., (2023) Impact of small intestinal bacterial overgrowth on symptoms and quality of life in irritable bowel syndrome. Journal of Digestive Diseases, 24(3):194-202. doi: 10.1111/1751-2980.13189. Epub 2023 Jun 8.
Popular Articles
View all Gut Health articles-
Gut Health15 Nov 2023
-
Gut Health14 Nov 2023
-
General Health06 Dec 2023