Probiotics for Acne & Skin Health
Gut health and skin health have been linked as far back as the early 20th century1. This article will look at the current understanding behind this link, especially the link between gut health and acne, and the role probiotics can play in this relationship.
Teenagers are not the only age group affected by pesky, painful spots and breakouts - acne is a common complaint amongst adults too. In this article we answer your questions about the link between gut health and skin health, and how probiotics might help:
- What causes acne and spots?
- How can gut health affect your skin and why?
- The skin microbiome
- Can probiotics help acne?
- Probiotics for rosacea
- Which are the best probiotics for skin health?
- Is it possible to develop acne after taking antibiotics?
- Probiotic skin care
- Five tips for healthy skin and a healthy gut
- Probiotics for acne and skin health: an overview
What causes acne and spots?
Acne is caused by inflammation of the skin, and particularly affects the sebaceous glands which produce sebum, the skin’s natural oil that keeps it lubricated. Excessive sebum and dead skin cells block skin follicles (appearing as blackheads). These blocked pores are breeding grounds for further infection and inflammation. Spots develop as papules (red bumps) and pustules (whiteheads). Although there are various factors that may trigger acne including hormonal, dietary and environmental factors, the impact of gut health should also be a major consideration.
How can gut health affect your skin and why?
A healthy gut is largely influenced by the health of the collection of microbes that live in our gut, known as the gut microbiome. The gut microbiome not only affects gut health locally but also has far-reaching effects around the body. It has been implicated in many common skin disorders such as eczema, psoriasis and acne2.
The gut can influence skin health through what is referred to as the gut-skin axis3. As 70% of our immune cells are found in the gut, our gut microbes can affect the function of immune cells. Ideally this results in an increase in the production of anti-inflammatory messengers (cytokines) and a reduction of the levels of pro-inflammatory cytokines. However, dysbiosis, an imbalance between friendly and more harmful bacteria in the gut, is frequently present in acne4 and can have negative effects on our immune responses. To learn more, you may like to read the article What is Dysbiosis?
In response to dysbiosis, inflammation or infection in the gut, the gaps between the cells lining the gut become larger, causing what is known as “leaky gut”. Beneficial gut bacteria, known as probiotics, inhibit the growth of harmful bacteria, or pathogens, and strengthen the gut wall lining5. But when overgrowths of pathogens damage the gut wall, the contents of the gut leak through this abnormally permeable lining, and can stimulate an immune cell response, triggering inflammation in the body which may contribute to the development of acne6. Bacterial by-products can also pass through these gaps in the gut wall lining, through the bloodstream to the skin3 where they can dry and harden the skin7.
.png)
The skin microbiome
Like the gut, the skin is colonised by its own collection of microbes called the skin microbiome. Common bacteria normally found on the skin include Staphylococci, Corynebacteria, Propionibacterium, Brevibacterium and Micrococci8. The skin microbiome composition varies from person to person based on factors such as age, gender and environment.
Colonisation of the skin with the bacteria Propionibacterium acnes is associated with acne8 and can trigger an inflammatory reaction. The first line treatment for acne vulgaris is antibiotics. Unfortunately, there has been an increase in antibiotic resistant strains of Propionibacterium acnes in recent years9 and antibiotics may cause unpleasant side effects. Those who suffer with acne may find themselves looking for alternative options such as probiotics to help manage their acne, or to ameliorate the side effects of antibiotic medication – read more about this below.
Can probiotics help acne?
There is a growing interest in the use of probiotics for acne and other skin conditions, but how might they help? Let’s look at the different ways in which they might have a benefit.
- Reduce inflammation – Acne is an inflammatory condition, and Lactobacilli and Bifidobacteria strains have been shown to reduce the release of pro-inflammatory cytokines, TNF- α, IL-6 and IL-8 and increase the release of anti-inflammatory cytokines, IL-1010,11,12.
- Reduce oxidative stress - The body naturally produces what are called free radicals as a result of metabolic processes in the body. Antioxidants that we consume in our diets, for example in brightly coloured fruit and vegetables, counteract these free radicals. However, there is often an imbalance with too many free radicals produced and not enough antioxidants to counteract their effects, and this is called oxidative stress. This excess of free radicals contributes to inflammation. In acne, there is an increase in oxidative stress and markers of oxidative stress such as hydroperoxide. These markers of oxidative stress including hydroperoxide have also been reduced by specific probiotics strains11.
- Rebalance gut dysbiosis – Probiotic supplementation can rebalance the gut microbiome by boosting the levels of beneficial bacteria and inhibiting the growth of more harmful bacteria. Find out more by reading the microbiome – all you need to know.
- Inhibit pathogenic bacteria on the skin – Natural bacterial inhabitants of the skin include Staphylococcus epidermidis and Streptococcus salivarius, both of which can inhibit the growth of Propionibacterium acnes13. Although currently these probiotic strains are not available for skin care, the pharmaceutical company, Bayer announced their plans to develop a natural skincare range containing Staphylococcus epidermidis in the near future14.
- Maintain gut barrier integrity – Increased intestinal permeability, otherwise known as “leaky gut”, can contribute to the development of acne2. Probiotics can reinforce the lining of the gut wall and inhibit the growth of pathogens that damage the delicate gut lining.
- Promote gut health and regulate bowel movements – Individuals with acne are more likely to suffer with regularity and digestive issues15 Dysbiosis and “leaky gut” are seen more frequently in those suffering with bowel irregularity, compared with healthy individuals16 both of which may contribute to the development of acne.
- Help to manage the effects of stress – There is a link between mental health, the gut, and skin health, known as the gut-skin-brain axis. Mental health issues such as anxiety and depression occur frequently alongside chronic skin conditions such as acne17, and stress is an important trigger of acne18. In the stress response, cortisol, our main stress hormone, is released into the bloodstream. It can bind to receptors in the skin resulting in increased sebum production and inflammation. Stress can also trigger acne indirectly by causing dysbiosis in the gut19. This upset to the gut microbiome can increase intestinal permeability causing “leaky gut” leading to inflammation2. Both dysbiosis and “leaky gut” can contribute to the development of acne and can be improved by probiotics as discussed above. To learn more about the relationship between the gut and mental health, read these articles: The gut-brain axis and Probiotics for Stress.
Probiotics for rosacea?
Rosacea, a skin condition that causes blushing, small bumps and visible blood vessels on the face, is often mistaken for acne. However, redness associated with acne tends to be located around individual spots anywhere on the face or body, while rosacea skin flushing more commonly occurs in the centre of the face.
There may be links between the gut and rosacea. A large clinical study in Denmark29 found that a high number of adults diagnosed with rosacea also had gastrointestinal disorders such as Crohn disease, ulcerative colitis, and IBS.
Read on for more information about the best probiotics for rosacea and other skin conditions.
Which are the best probiotics for skin health?
Currently, there are few clinical trials which directly assess the effects of specific strains of probiotics on skin health. However, there are several clinically researched probiotic strains that may help by addressing some of the triggers for acne.
Bifidobacterium lactis HN019
Bifidobacterium lactis HN019 can help address gut-related triggers of acne by helping to improve the health of the gut microbiome, reduce inflammation and manage occasional constipation.
- To demonstrate its positive effects on gut health, Bifidobacterium lactis HN019 was given daily for 4 weeks. In the probiotic group, the composition of the gut microbiome was greatly improved compared to placebo. Significant increases of good bacteria, Bifidobacteria, Lactobacilli and Enterococci, were seen, and levels of pathogenic Enterobacteria were reduced20.
- This strain has also shown potential to reduce inflammation. Results from another study showed significant reductions of inflammatory messengers and markers of oxidative stress were noted following daily supplementation with Bifidobacterium lactis HN019 for 90 days11.
- In individuals with less than 3 bowel movements a week, Bifidobacterium lactis HN019 was found to significantly increase bowel movement frequency21.
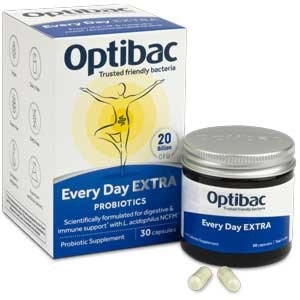
Find Bifidobacterium lactis HN019 in Optibac Probiotics Every Day MAX
Bifidobacterium lactis Bi-07 ®
- This strain has been shown to reduce the severity of Atopic Dermatitis (AD), an increasingly common chronic inflammatory skin disease, in children.
- In one clinical trial27 50 children with AD were given either a placebo, or a probiotic supplement containing either Lactobacillus acidophilus NCFM® or Bifidobacterium lactis Bi-07®. A measurable reduction in the severity of AD was observed in the Bi-07 group.
Lactobacillus acidophilus NCFM ®
- Lactobacillus acidophilus was one of the first probiotic bacteria to be used to help with acne. In one of the first ever clinical studies assessing the effects of probiotics on skin health, milk containing Lactobacilli was noted to improve the severity of acne13.
- It has also been shown to minimise the negative effects of antibiotics on gut microbiome composition23.
- Lactobacillus acidophilus NCFM ® may contribute to improved gut health and in turn skin health by improving regularity and preventing dysbiosis.
- Lactobacillus acidophilus NCFM ® in combination with Bifidobacterium lactis HN019 has been shown to be increase the number of bowel movements per week22.
Lactobacillus acidophilus NCFM ®. can be found in Optibac Probiotics Every Day EXTRA
For information about the best strains for babies and children with skin problems, read these articles: Baby Probiotics and Probiotics for Kids.
Is it possible to develop acne after taking antibiotics?
Although they are often prescribed to treat persistent acne, antibiotics can deplete the natural friendly bacteria living in the gut resulting in dysbiosis and inflammation24, both potential contributing factors in the development of acne. To help support the gut when taking antibiotics, consider a probiotic supplement researched for use during and after antibiotic therapy such as Lactobacillus acidophilus NCFM® which has been shown to restore balance in the gut microbiome after antibiotic treatment.
To learn more about protecting the gut when taking antibiotics, read this article about taking probiotics with antibiotics.
Probiotic skin care
In recent years, probiotic skin care has become popular under the premise that applying probiotics directly to the skin will positively affect the local skin microbiome. Whilst to date there have not been many clinical trials looking at topical probiotics for skin conditions, research so far suggests that they may prevent growth of harmful bacteria implicated in acne such as Propionibacterium acnes6.
One exciting study that came to light in early 2022 found that a topical application of specific lactobacilli strains positively alters the skin microbiome and reduces acne lesions in people with mild-to-moderate acne28. Participants used a daily topical application of Lacticaseibacillus rhamnosus GG, Lactobacillus plantarum WCFS1, and Lactiplantibacillus pentosus KCA1 microencapsulated into a cream for 8 weeks. Researchers reported a significant reduction in inflammatory acne lesions at the end of the trial.
Lactobacillus rhamnosus LGG® can be found in Optibac Probiotics Babies & Children.
Five tips for healthy skin and a healthy gut
- Be mindful of dietary habits – The typical Western diet – high fat, high sugar, low fibre – has been linked with acne25. Consider incorporating more whole foods like fruit and vegetables and wholegrains.
- Drink plenty of water – Keeping hydrated is essential for bowel regularity and a heathy gut.
- Work up a sweat – Exercise may boost skin health by increasing blood flow and the excretion of waste products in sweat but research has also shown that exercise can reduce skin deterioration associated with aging26.
- Try a yoghurt face mask – Beauty experts use live natural yoghurt applied directly to the face and left for 10 to 15 minutes. The benefits of a yoghurt face mask may be because of the Lactobacilli probiotic bacteria commonly found in live yogurts.
- Consider a probiotic supplement – A daily probiotic supplement may help improve skin health by optimising gut health including strains such as Bifidobacterium lactis HN019 or Lactobacillus acidophilus NCFM ®. Both Bifidobacterium lactis HN019 and Lactobacillus acidophilus NCFM ® can be found in Optibac Probiotics Every Day MAX

Probiotics for acne and skin health: an overview:
- Our gut health plays an important role in our skin health.
- The gut microbiome influences our skin health through its effects on our immune health and inflammation.
- Probiotics may positively impact skin health by helping to reduce inflammation, reduce oxidative stress, improve the composition of the gut microbiome, maintain a healthy gut environment, and manage the effects of stress.
- Probiotic strains that may help to address some of the triggers for acne include Bifidobacterium lactis HN019, Bifidobacterium lactis Bi-07® and Lactobacillus acidophilus NCFM®.
- Further well-designed clinical trials are required to ascertain the best probiotic strains for acne and skin health.
If you enjoyed this article, you may also like to read:
What is the Best Probiotic Supplement for Women? and Probiotics for Your Family’s Immunity
Healthcare professionals can visit the Probiotics Database to learn more about Lactobacillus acidophilus NCFM ®.
To learn more about how probiotics can help with eczema, health professionals can read this article on the Probiotic Professionals site: Probiotics for Eczema.
To learn more, health professionals can read this article on the Professionals site: Probiotics for constipation.
References
- Gordon S. Elie Metchnikoff: Father of natural immunity. Eur J Immunol. 2008;38(12):3257-3264. doi:10.1002/eji.200838855
- Salem I, Ramser A, Isham N, Ghannoum MA. The gut microbiome as a major regulator of the gut-skin axis. Front Microbiol. 2018;9(JUL):1-14. doi:10.3389/fmicb.2018.01459
- O’Neill CA, Monteleone G, McLaughlin JT, Paus R. The gut-skin axis in health and disease: A paradigm with therapeutic implications. BioEssays. 2016;38(11):1167-1176. doi:10.1002/bies.201600008
- Yan HM, Zhao HJ, Guo DY, Zhu PQ, Zhang CL, Jiang W. Gut microbiota alterations in moderate to severe acne vulgaris patients. J Dermatol. 2018;45(10):1166-1171. doi:10.1111/1346-8138.14586
- Krishna Rao R, Samak G. Protection and Restitution of Gut Barrier by Probiotics: Nutritional and Clinical Implications. Curr Nutr Food Sci. 2013;9(2):99-107. doi:10.2174/1573401311309020004
- Bowe WP, Patel NB, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis: From anecdote to translational medicine. Benef Microbes. 2014;5(2):185-199. doi:10.3920/BM2012.0060
- Miyazaki K, Masuoka N, Kano M, Iizuka R. Bifidobacterium fermented milk and galacto-oligosaccharides lead to improved skin health by decreasing phenols production by gut microbiota. Benef Microbes. 2014;5(2):121-128. doi:10.3920/BM2012.0066
- Grice, Elizabeth A. (Genetics and Molecular Biology Branch, National Human Genome Research Institute, National Institutes of Health, Bethesda, Maryland, 20892–4442 U., Segre JA. The skin microbiome. Nat Rev Microbiol. 2013;9(4):244-253. doi:10.1038/nrmicro2537.The
- Dreno B, Thiboutot D, Gollnick H, et al. Antibiotic stewardship in dermatology: Limiting antibiotic use in acne. Eur J Dermatology. 2014;24(3):330-334. doi:10.1684/ejd.2014.2309
- Azad MAK, Sarker M, Wan D. Immunomodulatory Effects of Probiotics on Cytokine Profiles. Biomed Res Int. 2018;2018. doi:10.1155/2018/8063647
- Bernini LJ, Simão ANC, De Souza CHB, et al. Effect of Bifidobacterium lactis HN019 on inflammatory markers and oxidative stress in subjects with and without the metabolic syndrome. Mineral Mag. 2018;120(6):645-652. doi:10.1017/S0007114518001861
- Cosseau C, Devine DA, Dullaghan E, et al. The commensal Streptococcus salivarius K12 downregulates the innate immune responses of human epithelial cells and promotes host-microbe homeostasis. Infect Immun. 2008;76(9):4163-4175. doi:10.1128/IAI.00188-08
- Goodarzi A, Mozafarpoor S. The potential of probiotics for treating acne vulgaris : A review of literature on acne and microbiota. 2020;(February). doi:10.1111/dth.13279
- Bayer to develop skin care from bacteria strains. https://www.cosmeticsdesign.com/Article/2020/01/14/Bayer-to-develop-skin-care-from-bacteria-strains. Accessed June 5, 2020.
- Zhang H, Liao W, Chao W, et al. Risk factors for sebaceous gland diseases and their relationship to gastrointestinal dysfunction in Han adolescents. J Dermatol. 2008;35(9):555-561. doi:10.1111/j.1346-8138.2008.00523.x
- Khalif IL, Quigley EMM, Konovitch EA, Maximova ID. Alterations in the colonic flora and intestinal permeability and evidence of immune activation in chronic constipation. Dig Liver Dis. 2005;37(11):838-849. doi:10.1016/j.dld.2005.06.008
- Silverberg J, Silverberg N. Epidemiology and extra-cutaneous comorbidities of severe acne in adolescence: A US population-based study. Br J Dermatol. 2014;170(5):1136-1142.
- Chen Y, Lyga J. Brain-skin connection: Stress, inflammation and skin aging. Inflamm Allergy - Drug Targets. 2014;13(3):177-190. doi:10.2174/1871528113666140522104422
- Bowe WP, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis - Back to the future? Gut Pathog. 2011;3(1):1. doi:10.1186/1757-4749-3-1
- Ahmed M. Impact of Consumption of Different Levels of Bifidobacterium Lactis HN019 on the Intestinal Microflora of Elderly Human Subjects - PubMed. J Nutr Health Aging. https://pubmed.ncbi.nlm.nih.gov/17315077/. Accessed June 1, 2020.
- Ibarra A, Latreille-Barbier M, Donazzolo Y, Pelletier X, Ouwehand AC. Effects of 28-day Bifidobacterium animalis subsp. lactis HN019 supplementation on colonic transit time and gastrointestinal symptoms in adults with functional constipation: A double-blind, randomized, placebo-controlled, and dose-ranging trial. Gut Microbes. 2018;9(3):236-251. doi:10.1080/19490976.2017.1412908
- Magro DO, De Oliveira LMR, Bernasconi I, et al. Effect of yogurt containing polydextrose, Lactobacillus acidophilus NCFM and Bifidobacterium lactis HN019: A randomized, double-blind, controlled study in chronic constipation. Nutr J. 2014;13(1):1-5. doi:10.1186/1475-2891-13-75
- Engelbrektson A, Korzenik JR, Pittler A, et al. Probiotics to minimize the disruption of faecal microbiota in healthy subjects undergoing antibiotic therapy. J Med Microbiol. 2009;58(5):663-670. doi:10.1099/jmm.0.47615-0
- Yoon MY, Yoon SS. Disruption of the Gut Ecosystem by Antibiotics. Yonsei Med J. 2018;59(1):4-12. doi:10.3349/ymj.2018.59.1.4
- Bowe WP, Joshi SS, Shalita AR. Diet and acne. J Am Acad Dermatol. 2010;63(1):124-141. doi:10.1016/j.jaad.2009.07.043
- Crane JD, Macneil LG, Lally JS, et al. Exercise-stimulated interleukin-15 is controlled by AMPK and regulates skin metabolism and aging. Aging Cell. 2015;14(4):625-634. doi:10.1111/acel.12341
- Gobel et al., (2010). ‘Probiotics to young children with atopic dermatitis: A randomized placebo-controlled trial’. International Journal of Probiotics and Prebiotics, 5(2):53-59.
- Lebeer S et al., (2022) Selective targeting of skin pathobionts and inflammation with topically applied lactobacilli. Cell Reports Medicine, 3(2) DOI:https://doi.org/10.1016/j.xcrm.2022.100521
- Egeberg A et al., (2016) Rosacea and gastrointestinal disorders: a population-based cohort study. British Journal of Dermatology, 176(1):100-106. doi: 10.1111/bjd.14930.
- Huuskonen L, et al. (2022) Effects of Bifidobacterium animalis subsp. lactis Bl-04 on Skin Wrinkles and Dryness: A Randomized, Triple-Blinded, Placebo-Controlled Clinical Trial. Dermato. 2022; 2(2):30-52. https://doi.org/10.3390/dermato2020005
Popular Articles
View all General Health articles-
General Health10 Nov 2023
-
General Health06 Nov 2023
-
General Health13 Feb 2024


