The Best Probiotics for IBS
Could probiotics help with your IBS symptoms? In this article, we’ll explore their benefits, how to choose the best probiotic, and what to look for in a supplement. If you're short on time, watch my short IBS information video for a guide on how to choose the best probiotics for IBS and your IBS type.
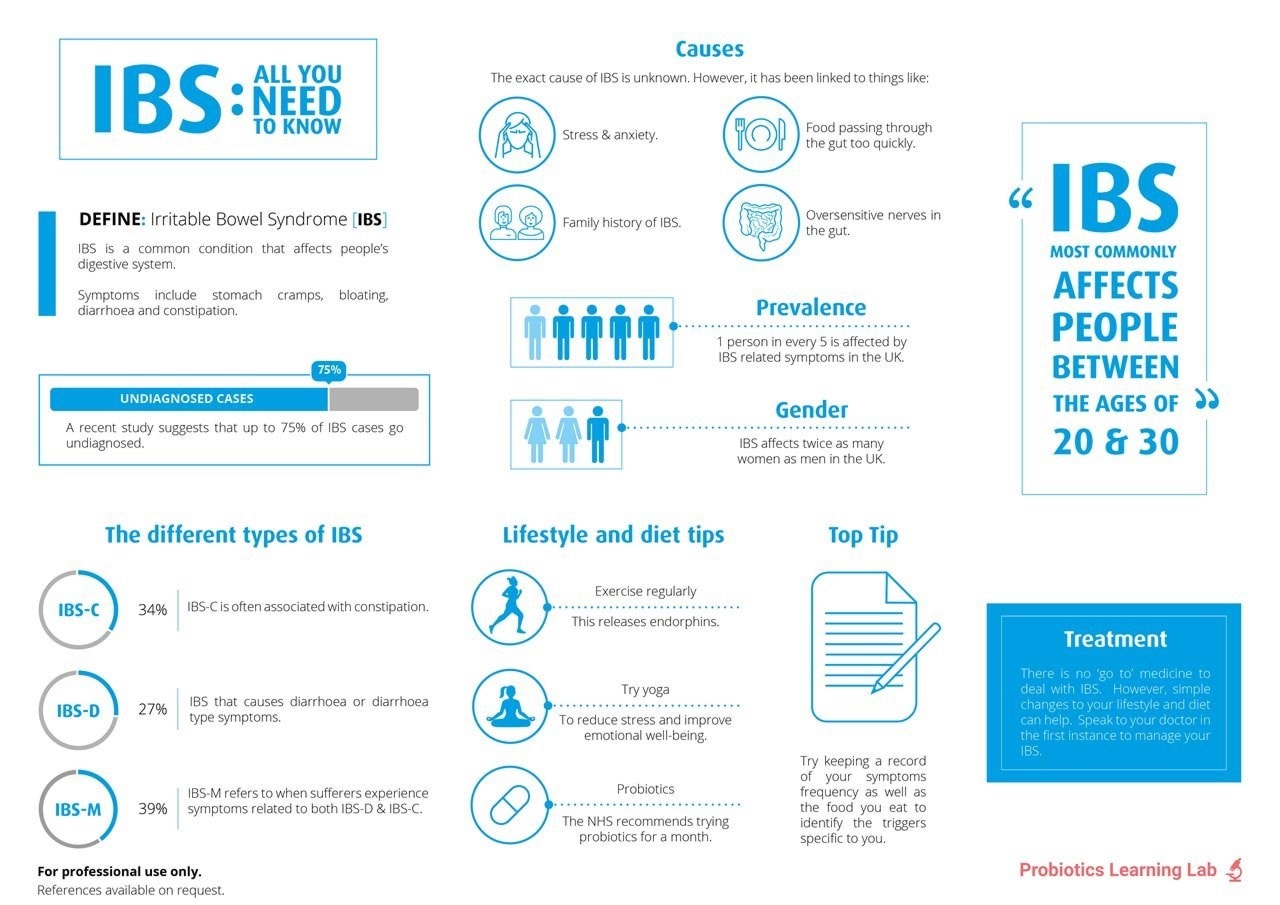
Irritable Bowel Syndrome (IBS) is a common digestive disorder affecting up to 20% of the UK population, with women twice as likely to be affected as men. While there’s no known cure or single cause, IBS treatment focuses on managing symptoms, which vary from person to person. Certain foods—such as wheat, dairy, and high-FODMAP foods - along with stress and gut bacteria imbalances5, may trigger or worsen symptoms.
Many find relief through diet and lifestyle changes, making it helpful to track food and symptoms over time. Natural supplements, particularly probiotics for IBS have also gained popularity as a go-to option.
In the video below, I share the best probiotic strains for the most common types of IBS.
Which probiotics are best for IBS?
IBS presents a range of symptoms, so choosing probiotics with well-researched strains suited to your needs is key. A high-quality daily probiotic can also support overall gut health alongside targeted strains for specific IBS types.
Best 'all-round' strain for IBS:
Lactobacillus acidophilus NCFM® is an excellent choice, shown to help with:
- Abdominal discomfort
- Gas/Bloating
- Poor gut motility
- Loose stools
- Bowel regularity
Research15,29 confirms this strain benefits all IBS types, making it a valuable addition to daily probiotic support.
Targeted strains28 researched in specific IBS symptoms:
- IBS-D – Diarrhoea predominant & post-infectious IBS - Saccharomyces boulardii
- IBS-C – Constipation predominant - Bifidobacterium lactis BB-12®
IBS is classified under the Rome criteria into:
- IBS-D – Diarrhoea predominant
- IBS-C – Constipation predominant
- IBS-A – Alternating constipation & diarrhoea
- IBS-U – Unspecified & varying symptoms
- Post-infectious IBS
For more on IBS, read our information sections below:
- Do probiotics help IBS?
- Can probiotics make IBS worse?
- Prebiotics for IBS
- NHS recommends probiotics for IBS
Please note: if you are experiencing severe IBS symptoms, you must always speak to your doctor for advice.
Do probiotics help IBS?
Many people ask, “Can probiotics help IBS?” or “Should IBS sufferers take probiotics?” Research suggests they can, with numerous clinical trials showing benefits for IBS symptoms. Even the NHS recommends probiotics for IBS, as they are generally safe, natural, and can be taken alongside most prescription and over the counter medications for IBS. However, if you suspect IBS, always consult a doctor for a proper diagnosis.
IBS is linked to an imbalance in the gut microbiome5, where harmful bacteria can outweigh beneficial ones. Read more about the gut microbiome in All About the Microbiome. Studies suggest a connection between IBS-D and the presence of Brachyspira bacteria22, while IBS sufferers often have lower levels of beneficial Bifidobacterium species and higher levels of harmful Clostridium bacteria.
Taking a high quality probiotic may help:
- Increase good bacteria, reducing space for harmful microbes
- Aid digestion, helping break down foods that may trigger IBS symptoms
- Support stress management, as a balanced gut microbiome may help reduce the impact of stress on the gut
When choosing a probiotic supplement for IBS, for best results select probiotics with strains clinically tested in IBS sufferers, rather than just lab studies. Each strain has unique properties with different probiotics benefiting specific symptoms such as bloating, diarrhoea, or constipation.
Can probiotics make IBS worse?
Probiotics are natural and well-tolerated by most people. However, if your gut microbiome is severely imbalanced, known as dysbiosis, you may experience temporary digestive changes when first introducing probiotics. These effects typically subside within 48 hours as your gut adjusts, though in some cases, it may take a little longer.
If discomfort arises, try:
- Lowering the dose and gradually increasing it
- Taking a short break before reintroducing probiotics
Probiotics with prebiotics may also cause temporary bloating or gas, particularly in those sensitive to certain carbohydrates. If following a low FODMAP diet, prebiotic or synbiotic supplements are usually avoided during this phase. Once your gut adjusts, probiotics can begin to support a healthier balance of bacteria and overall digestive well-being.
Probiotics for IBS-D
If your doctor diagnoses you with IBS and your primary symptom is diarrhoea, then you have IBS-D. Saccharomyces boulardii is one of the best probiotics for IBS-D symptoms.
This unique probiotic is in fact a yeast, the only yeast 'friendly' enough to be called a probiotic.S. boulardii has over 50 years of research supporting its use, and is recommended in many hospitals worldwide for diarrhoea. A 2021 review of 42 clinical trials confirmed S. boulardii as one of the best probiotic strains for IBS diarrhoea27. The review showed that S. boulardii offered significant improvements in abdominal pain and frequency of bowel movements for individuals with IBS-D. As well as IBS-D, it has also been shown to be beneficial for diarrhoea associated with Inflammatory Bowel Disease (IBD), antibiotic-associated diarrhoea and traveller’s diarrhoea. Healthcare practitioners can read more about probiotics for IBD on the Probiotic Professionals site.
As S. boulardii is a friendly yeast, it has very different properties to friendly bacteria; it's a 'transient' probiotic meaning that it does not colonise for long in the gut. Therefore it’s a good idea to take a probiotic containing colonising friendly bacteria alongside S. boulardii as they work together. For this, use one of the probiotic strain recommendations in the IBS-A section.
The probiotic strains Pediococcus acidilactici CECT 7483, Lactobacillus plantarum CECT 7484 and Lactobacillus plantarum CECT 7485 have also been researched and shown to be good probiotics for IBS-D13. This trial measured improvements in the quality of life of the participants, in relation to their IBS diarrhoea symptoms, which is thought to be one of the most accurate ways of measuring the effectiveness of the treatment.

Probiotics for IBS-C
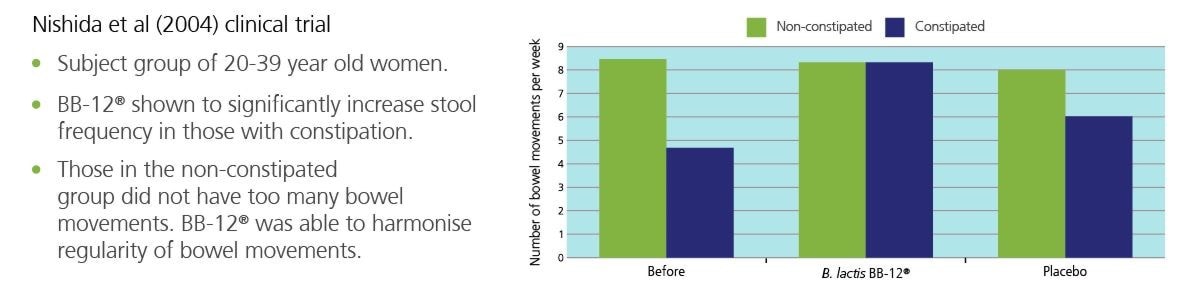
If you have IBS which presents with regularity issues and constipation, this is known as IBS-C. There are a couple of probiotic strains which have been particularly researched for constipation: Bifidobacterium lactis BB-12® and Bifidobacterium lactis HN019. Bifidobacteria like to live in the large intestine where the stool is formed, so they tend to be the most researched probiotics for regularity issues.
Bifidobacterium lactis BB-12®, is thought to be the most well-researched strain in the whole Bifidobacteria family, and has been particularly researched in those with constipation3,4. It promotes more regular bowel movements, which are easier to pass, as well as supporting gut health in general.
In one clinical trial, over 100 women with constipation were given a supplement containing Bifidobacterium lactis BB-12® and prebiotics14.Those who took the B. lactis BB-12® supplement were no longer constipated and had normal bowel movements compared to those who took the placebo.
The illustrated clinical trial used Bifidobacterium lactis BB-12® in combination with a prebiotic; however, prebiotics don't suit everyone who suffers from IBS. Read more about prebiotics and IBS below.
The probiotic strain Bifidobacterium lactis HN019 has been researched for all symptoms of IBS, and has also been shown to improve bowel regularity10. IBS-C sufferers who prefer to avoid prebiotics may get on better with a supplement containing Bifidobacterium lactis HN019 without added prebiotics.
Healthcare professionals can learn more about using probiotics for constipation on the Probiotic Professionals site, and read the rest of the research involving Bifidobacterium lactis HN019 on the Probiotics Database.
Probiotics for IBS-A (also known as IBS-M)
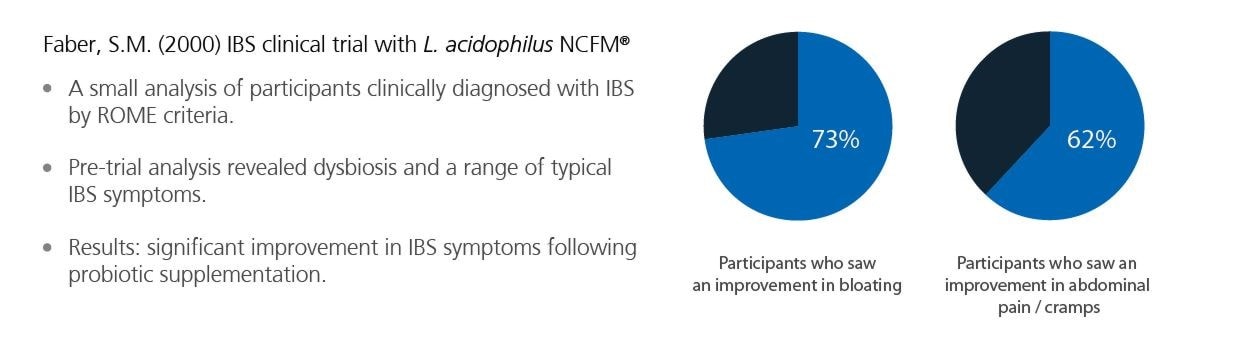
Many people with this type of the condition find they have alternating symptoms of IBS diarrhoea, bloating, pain, and constipation. This form of IBS is known as IBS-A (alternating) or IBS-M (mixed symptoms). For the relief of this IBS variant, it can be hard to know which symptom to target, but the best first step is to try a high-quality, general, daily probiotic for all-round gut-support, as an imbalanced gut bacteria populations are thought to be a factor in all types of IBS5. Two strains, Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07® have been specifically trialled in those with IBS and found to not only regulate bowel movements29 but also for the relief of IBS bloating, abdominal distension, and abdominal cramps15. Even on its own Lactobacillus acidophilus NCFM® has been shown to be effective in improving various symptoms of patients with IBS5,6.
Healthcare professionals can read more about Bifidobacterium lactis Bi-07® on the Probiotics Database.
Whilst Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07® are the most recommended strains for all-round IBS support, there a few other probiotic strains which can be considered:
The probiotic strain Bacillus coagulans Unique IS-2 strain has been studied for the support of IBS symptoms in both adults and children. In one study involving 136 adults with IBS were given B. coagulans Unique IS-2 for eight weeks. A significant reduction in abdominal pain and an increase in the number of complete spontaneous bowel movements was noted, compared with placebo26.
Bifidobacterium infantis 35624, also known as 'Bifantis’, has been researched in those with Irritable Bowel Syndrome with positive results8. An 8-week trial with 75 participants associated B. infantis 35624 with a reduction in pain, discomfort, bloating and constipation. Healthcare practitioners can refer to Bifidobacterium infantis 35624, which has more information on this strain.
A specific strain of the Lactobacillus plantarum species (L. plantarum Lp299v®) has also been clinically trialled on participants with IBS diarrhoea, bloating, and constipation and shown to reduce IBS symptoms16. A 4-week clinical trial of 60 IBS sufferers showed that those in the probiotic group had a decrease in flatulence and pain and more consistent bowel movements. Healthcare practitioners can visit this page on the Probiotics Database L. plantarum Lp299v® to find out more about related research.
Additionally, in a study involving 75 healthy volunteers experiencing stress, supplementation with Lactobacillus helveticus Rosell-52 and Bifidobacterium longum Rosell-175 over a 3-week period was associated with reductions in stress-induced gastrointestinal symptoms, including abdominal pain and nausea/vomiting, with a trend toward decreased flatulence and gas production37.
Probiotics for IBS-U
If the previous types of IBS do not sound quite like you, then you might be struggling with IBS-U (Undefined or Unclassified). This form of IBS is characterised by a stool consistency that doesn't fit into the other categories.Sufferers may experience both loose, watery stools and harder stools, but both less than 25% of the time. This IBS type tends to be less common than the others but has similar causes, including diet or an imbalance of bacteria in the gut and bowels. There is also evidence to suggest a gut-brain connection17.
Again, as with IBS-A/M above, it's best to begin supporting this type of IBS with probiotic strains which have been shown to help with a variety of symptoms, such as Lactobacillus acidophilus NCFM® and Bifidobacterium lactis Bi-07®. After supplementing with these strains for a month or so, symptoms may improve fully, or begin to trend more towards one symptom, then it will be possible to add in more specific strains for more targeted support. It's also wise to consider triggers so keeping an IBS symptom diary can be helpful.
Post-infectious IBS
Approximately one in ten people who suffer from IBS believe their symptoms began with an upset stomach. Serious infections such as gastroenteritis or parasitic infections are more likely to cause this sort of IBS18. It seems that there are a couple of risk factors for developing post-infectious IBS, including the duration of the illness, whether you are a smoker, female, suffer from depression, or experienced any adverse life events three months previously19.
If you have this type of IBS, you are more likely to suffer from diarrhoea or a mixed stool pattern. Taking the probiotic yeast Saccharomyces boulardii can help address the cause of the infectious illness30 itself and also support the IBS symptoms afterwards. It may also be prudent to take a general probiotic (see the strains recommended in the IBS-A section) alongside S. boulardii for all-round gut support.
At the end of the day, everyone is different, and IBS bloating sufferers will have different gut floras to one another. With probiotics, it is often a case of trial and error to find which species and strains work for that individual. There is no harm, in 'mixing and matching' different products if this works for you. You can't take 'too many' probiotics. For more information on this topic, see Is it possible to overdose on probiotics?

Prebiotics for IBS
If you experience bloating or digestive discomfort when eating particular prebiotic foods, you may be wondering whether to choose a prebiotic or probiotic for IBS, or a combination called a synbiotic without irritating your gut.
If you’re highly sensitive to foods that fall into the high FODMAP category, such as garlic, onions, apples, and leeks, I firstly recommend working with a professional to try a low FODMAP diet to help calm your gut. During the elimination phase (which should only be a total of 4 weeks) you will be advised to avoid most prebiotic supplements.
For those who are mostly fine with prebiotic foods, which prebiotic supplements for IBS are best? Well, research shows that high dose synbiotic supplements including Fructooligosaccharides (FOS) were superior to placebo in improving bowel symptoms and fatigue in those with IBS20. Prebiotics for IBS-C can be supportive as FOS is a source of soluble fibre that adds bulk and absorbs water to help soften the stool, it also helps encourage peristalsis which is the movement of food through the gut. Prebiotics, such as FOS, are food for your gut bacteria and significantly increase levels of Bifidobacteria in those with IBS21. If you’re worried that introducing prebiotics for IBS will cause bloating, start low and slow! Taking them in the evening before bed can help too.
Learn more about prebiotics, prebiotic foods, and FODMAP diets by reading: What are prebiotics?
NHS recommendation on probiotics for IBS
The NHS recognises probiotics as a potential aid for helping relieve IBS symptoms23,31, stating on the NHS website that: "Probiotics may help reduce bloating and flatulence in some people with IBS." The NICE (National Institute for Health and Clinical Excellence) guidelines recommend trying probiotics for at least four weeks to manage IBS symptoms24.

A systematic review by Moayyedi et al. (2010) supported the effectiveness of probiotics25, contributing to their inclusion in NHS guidance. This marks a significant milestone, as probiotics are routinely prescribed in many European hospitals but were not always part of NHS recommendations.
IBS places a major burden on healthcare, costing the NHS £1.2–£2 billion per year according to a 2022 report34. With NHS online suggesting that 75% of people managing IBS through self-care, probiotics offer a natural and accessible option for symptom relief.
If you enjoyed this article, you may also like to read:
References
- Das S, et al. (2016) Efficacy and Safety of Saccharomyces boulardii in Acute Rotavirus Diarrhea: Double Blind Randomized Controlled Trial from a Developing Country. J Trop Pediatr. Dec;62(6):464-470
- Wan CM, et al (2017) A multicenter randomized controlled study of Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea in infants and young children. 4;55(5):349-354.
- Eskesen, D. et al. (2015), ‘Effect of the probiotic strain Bifidobacterium animalis subsp. lactis BB-12® on defecation frequency in healthy subjects with low defecation frequency and abnormal discomfort: a randomised, double-blind, placebo-controlled, parallel-group trial’, British Journal of Nutrition, Nov 28: 114(10) :1638–1646.
- Nishida, S. et al. (2004), ‘Effect of Yoghurt Containing Bifidobacterium lactis BB-12® on Improvement of Defecation and Fecal Microflora of Healthy Female Adults’, Milk Science, 53(2):71-80
- Faber, S.M. (2000) 'Treatment of abnormal gut flora symptoms in patients with irritable bowel syndrome'. Am J Gastroenterol 95(9):25333
- Lyra, A. et al., (2016) ‘Irritable bowel syndrome symptom severity improves equally with probiotic and placebo’. World Journal of Gastroenterology. 22 (48):10631–10642.
- O’Mahony L. et al (2005), ‘Lactobacillus and Bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles, Gastroenterology, 128(3):541-51.
- Whorwell PJ et al. (2006) 'Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome.' Am J Gastroenterol 101 7 1581-90.
- Ibarra, A. et al., (2018) ‘Effects of 28-day Bifidobacterium animalis subsp. lactis HN019 supplementation on colonic transit time and gastrointestinal symptoms in adults with functional constipation: A double-blind, randomized, placebo-controlled, and dose-ranging trial’. Gut Microbes, 9(3):236-251.
- Waller, P. A. et al., (2011) ‘Dose-response effect of Bifidobacterium lactis HN019 on whole gut transit time and functional gastrointestinal symptoms in adults’. Scandinavian Journal of Gastroenterology. 1057–1064
- Nobaek S. et al., (2000), ‘Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome’, Am. J. Gastroenterol. 95:1231-1238.
- Ducrotté P. et al., (2012). ‘Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome’. World Journal of Gastroenterology, 18:4012-4018.
- Lorenzo-Zúñiga V et al. (2014) I.31, a new combination of probiotics, improves irritable bowel syndrome-related quality of life. World J Gastroenterol 20 26 8709-16
- Malpeli, A. et al (2012) 'Randomised, double-blind and placebo-controlled study of the effect of a synbiotic dairy product on orocecal transit time in healthy adult women'. Nutr Hosp 27 4 1314-9.
- Ringel-Kulka, T. et al (2011) 'Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: a double-blind study'. J Clin Gastroenterol 45 6 518-25.
- Niedzielin K et al. (2001) 'A controlled, double-blind, randomized study on the efficacy of Lactobacillus plantarum 299V in patients with irritable bowel syndrome'. Eur J Gastroenterol Hepatol 13 10 1143-7.
- Mayer E, A. (2018). The Role of Gut-Brain Interactions in Influencing Symptoms of Irritable Bowel Syndrome. Gastroenterol Hepatol (N Y), 14(1):44–46.
- Lekha Saha. (2014). Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol.. 20 (22), 6759–6773.
- Robin Spiller, Klara Garsed. (2009). Postinfectious Irritable Bowel Syndrome. Gastroenterology. 136 (6), 1979-1988.
- Sang-Hoon Lee , Doo-Yeoun Cho , Seok-Hoon Lee , Kyung-Sun Han , Sung-Won Yan. (2019). A Randomized Clinical Trial of Synbiotics in Irritable Bowel Syndrome: Dose-Dependent Effects on Gastrointestinal Sympto. Korean J Fam Med. 1(40), pp.2-8. [Online]. Available at: 10.4082/kjfm.17.0064 [Accessed 19 May 2023].
- Bridgette Wilson, Megan Rossi, Eirini Dimidi, Kevin Whelan. (2019). Prebiotics in irritable bowel syndrome and other functional bowel disorders in adults: a systematic review and meta-anal. The American Journal of Clinical Nutrition. 109(4), p.1098–1111. [Online]. Available at: https://doi.org/10.1093/ajcn/nqy376 [Accessed 19 May 2023].
- Karolina S Jabbar, Brendan Dolan, Lisbeth Eklunde, Catharina Wising, Anna Ermund, Åsa Johansson, Hans Törnblom, Magnus Simren, Gunnar C Hansson. (2020). Association between Brachyspira and irritable bowel syndrome with diarrhoea. Gut. 0 (0), 1-13.
- NHS, 2017. NHS Choices. [Online] Available at: https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/diet-lifestyle-and-medicines/[Accessed 29 March 2018].
- NICE, 2017. NICE (National Institute for Health and Care Excellence). [Online] Available at: https://www.nice.org.uk/guidance/cg61/chapter/1-Recommendations[Accessed 29 March 2018].
- Moayyedi P, Ford AC, Talley NJ, et al. 2010 The efficacy of probiotics in the treatment of irritable bowel syndrome: a systematic review. Gut. 59(3):325-332. doi:10.1136/gut.2008.167270
- Madempudi, R. S. et al. (2019) ‘Randomized clinical trial: the effect of probiotic Bacillus coagulans Unique IS2 vs. placebo on the symptoms management of irritable bowel syndrome in adults’, Scientific Reports, 9(1). doi: 10.1038/s41598-019-48554-x.
- McFarland L, Karakan T, Karatas A (2021) Strain-specific and outcome-specific efficacy of probiotics for the treatment of irritable bowel syndrome: A systematic review and meta-analysis. eClinicalMedicine, 41: 101154
- Satish Kumar L, Pugalenthi L, Ahmad M, et al. (April 18, 2022) Probiotics in Irritable Bowel Syndrome: A Review of Their Therapeutic Role. Cureus 14(4): e24240. doi:10.7759/cureus.24240
- Magro, D.O., et al., (2014). ‘Effect of yogurt containing polydextrose, Lactobacillus acidophilus NCFM and Bifidobacterium lactis HN019: a randomized, double-blind, controlled study in chronic constipation’. Nutrition Journal, 13:75.
- Kirchhelle A. et al., (1996), ‘Treatment of persistent diarrhoea with Saccharomyces boulardii in returning travellers: results of a prospective study’. Fortschr. Med.114(11):136-140.
- NHS: (2018). Probiotics.[Online] https://www.nhs.uk/conditions/probiotics/ [Accessed 1st September 2022]
- Zhang J,Zheng H,Z Tao,Duan L, (2022) Effect of Microbiota-targeted Therapy on Gut Microbiota in Patients with Irritable Bowel Syndrome: A Scoping Review. Chinese General Practice.
- Shrestha B et al., (2022) The Role of Gut-Microbiota in the Pathophysiology and Therapy of Irritable Bowel Syndrome: A Systematic Review. Cureus, 14(8): e28064. doi:10.7759/cureus.28064
- https://www.practiceupdate.com/content/direct-healthcare-costs-of-ibs-in-the-uk/136874
- Chuah KH. et al., (2023) Impact of small intestinal bacterial overgrowth on symptoms and quality of life in irritable bowel syndrome. Journal of Digestive Diseases, 24(3):194-202. doi: 10.1111/1751-2980.13189. Epub 2023 Jun 8.
- Xie P et al., (2023) Outcome-Specific Efficacy of Different Probiotic Strains and Mixtures in Irritable Bowel Syndrome: A Systematic Review and Network Meta-Analysis. Nutrients; 15(17):3856. https://doi.org/10.3390/nu15173856
- Diop, L., Guillou, S., & Durand, H. (2008). Probiotic food supplement reduces stress-induced gastrointestinal symptoms in volunteers: a double-blind, placebo-controlled, randomized trial. Nutrition research (New York, N.Y.), 28(1), 1–5. https://doi.org/10.1016/j.nutres.2007.10.001
Popular Articles
View all Gut Health articles-
Gut Health16 Nov 2023
-
Gut Health07 Nov 2023
-
General Health15 Apr 2024