Child Microbiome: Dr Kate's Guide
It's never too late to start learning about your child's gut health. Make sure they get the best start in life, from birth to secondary school, by understanding how nurturing their gut microbiome can help optimise their overall health.
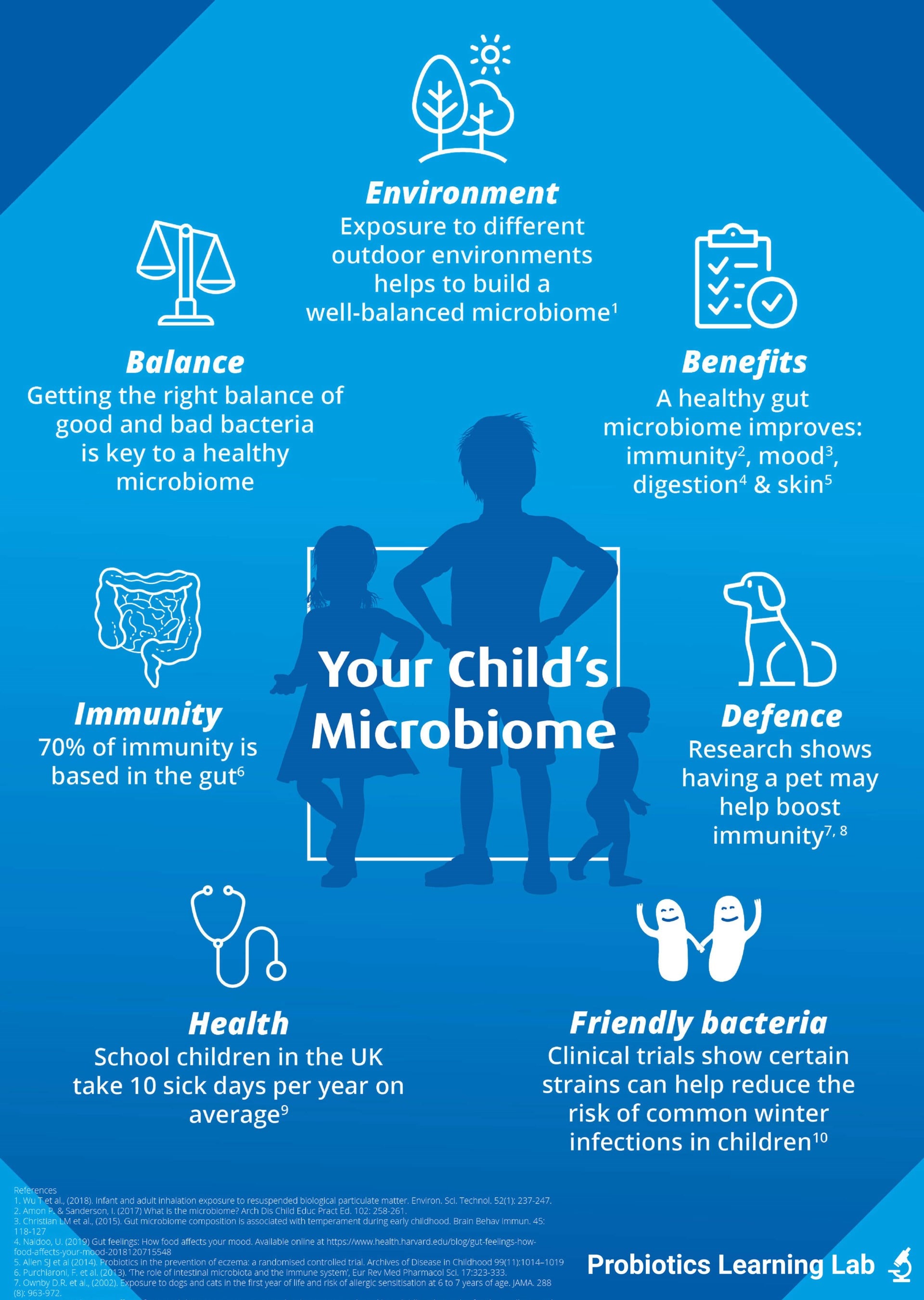
It may come as a surprise to some that the friendly bacteria living naturally inside your child's gut can influence various aspects of their health, including digestion, immune health, skin health and mental wellbeing. Your child's gut microbiome is established over the first few years of their life but it continues to change and adapt to their diet, lifestyle and environment. Continue reading to find out more about the factors that influence the health of your child's gut microbiome and how to keep it at its best.
Within this article:
- Your child’s microbiome timeline
- Toddlers
- Exposure to pets in early life can help build immunity later on
- Children
- Causes for gut dysbiosis in kids
- Summary
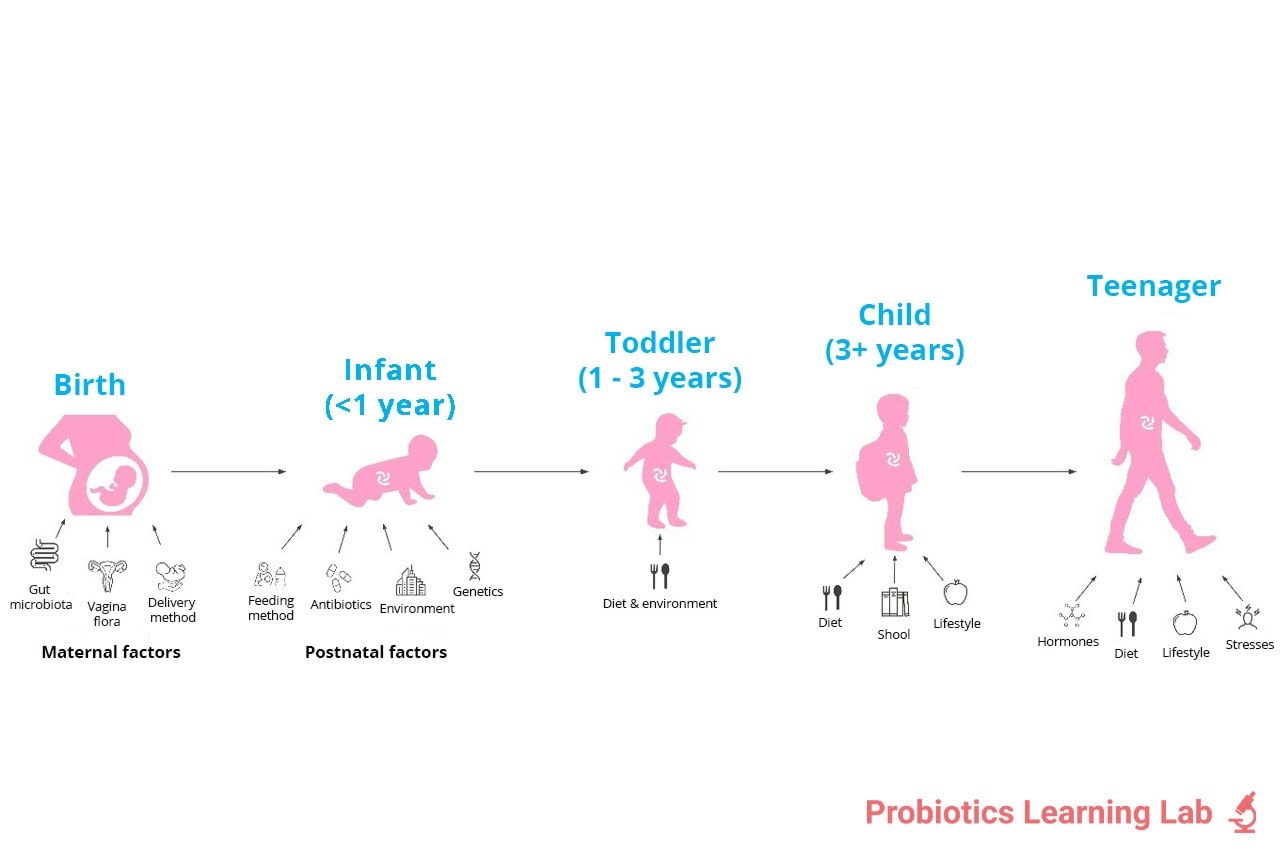
Your child’s microbiome timeline
Our childhood years are extremely important for all aspects of development. In particular, the foundations of our microbiome and immune system are formed.
Surprisingly, this all begins in the womb. Pregnancy and the first two years post-birth form the first 1000 days of life, and during this time we see major changes to the microbiome. These changes can affect both current and future health.
The microbiome composition tends to settle around age 3, however many factors can still disrupt the level of friendly bacteria. This may cause some unwanted side effects such as poor immunity, eczema, digestive issues or allergies (and many more).
Research suggests that friendly bacteria play a very important role in a child’s microbiome and overall health.
From the timeline above, you can see that many factors can impact the levels of friendly bacteria right from pregnancy and throughout childhood. We’re going to take a look at some of these factors in more detail over the course of the blog series.
This blog aims to focus on factors that particularly affect the microbiome of toddlers and children (age 2- 12).
Toddlers
We've all heard of the terrible twos! For toddlers, the microbiome and immune system are still learning and developing, so there are lots of experiences that continue to challenge their guts.
Nursery is one such experience that can throw a child’s microbiome into flux. This is a whole new world of other children and their microbes. Nurseries can be a breeding ground for harmful bacteria, with nearly two-thirds of children under 4 visiting their GP annually due to a cough1.
Whilst it’s likely that your child will get ill during the nursery years, you may be able to reduce the risk, severity and duration of illness by looking after their microbiome. Remember: 70% of the immune system resides in the gut, so a healthy gut microbiome is key for good immune health.
To help support their microbiome, you may choose to supplement with a probiotic that has been extensively trailed on infants and very young children like Bifidobacterium breve M-16V®. This strain has been shown to help support gut and immune health and can be found in Optibac Probiotics Baby Drops.
Exposure to pets in early life can help build immunity later on

As toddlers get older, they also start having more interactions with animals and foreign environments. Worried about germs from pets? Actually, one study investigated 474 children over a seven-year period. They found that children exposed to a pet in the first few years of life experienced a protective effect against eczema and allergies throughout childhood2. Talk about man’s best friend!
There is also some evidence that living on a farm may reduce the risk of allergy development in childhood, extending into adulthood4,5. However, it should be noted that evidence on animal interaction and gut health is still emerging and there are some inconsistencies.
Another interesting area in which the gut microbiome plays a role is a toddler’s behaviour. A study in 2015 demonstrated that toddlers who were more engaged, happy and interactive had a wider diversity of microbes in the gut and more Bifidobacteria6,7. This indicates that a healthy gut microbiome may be positively associated with mood. This connection is known as the gut-brain axis (and it's a favourite of mine). See how it is all connected?
Children
After the toddler years, the microbiome tends to stabilise; the foundations are pretty much formed. However, it can still be influenced by numerous lifestyle factors which may affect your child’s health and happiness.
When levels of friendly bacteria are reduced, this can cause dysbiosis (a microbial imbalance). You may not realise your child has dysbiosis, but it can cause some recognisable symptoms such as:
- Diarrhoea
- Constipation
- Low energy/fatigue & poor concentration
- Low mood
- Constant colds & flu
- Bloating
- Eczema & allergies
- Asthma
If your child is suffering from any of the above, it might be worth considering if it's down to poor gut health, and speaking to a doctor if symptoms persist.
Causes for gut dysbiosis in kids
Mental health
Stress, anxiety and depression are pretty common in adults, but we’re also seeing children (from primary age) are at increasingly higher risks of suffering with their mental wellbeing, too.
Low mood can impact the level of friendly bacteria in the gut microbiome, plus result in inflammation in the body if experienced on a long-term basis. Poor mental health can also affect immune health - have you noticed when you or your child are stressed, you’re both more likely to catch a cold?
There are a lot more reasons these days why children might feel stressed or anxious. They are under more pressure to perform at school and many do lots of extra-curricular activities on top of homework and school tests. There are also more social pressures to navigate today, especially with the rise in social media platforms which can open the door to cyberbullying.
Encourage your child to take a break occasionally, to go outside and play or read a book. Find ways to manage their stress, even if it’s something as simple as a day out with the family or a cuddle with mum or dad. Perhaps ask your school what they can do; for example, mindfulness classes are being looked at in many primary settings.
Antibiotics
Antibiotics are the most commonly prescribed medication given to children8. Unfortunately, they can be extremely damaging to the gut microbiome. Antibiotics are not always selective and they can wipe lots of good bacteria as well as the harmful ones causing the infection. This can cause short-term side effects, but antibiotic use (especially repeated prescriptions) may even result in future health issues.
In the short-term, dysbiosis occurs which explains why your child might develop diarrhoea or thrush from their course of antibiotics.
A very large study, including 142,824 children aged 3-18, found that extensive antibiotic use throughout children increased the risk of weight gain9. Lots of exposure in early years can also increase the risk of antibiotic resistance, which may limit future use of antibiotics.
If your child needs antibiotics then they should take them, but you might consider giving them specially formulated probiotics for kids too, to help top up their levels of good gut bacteria again.

Diet
Another cause of dysbiosis could be diet. It’s not always easy for busy parents to provide five portions of fruit and vegetables daily, but these foods can really enrich the microbiome and enhance gut health.
Lots of fruits and vegetables contain fibre, which encourages a balanced gut microbiome filled with lots of friendly bacteria. Specialised fibres known as prebiotics can even further support the growth of good bacteria. Plus, when friendly bacteria ferment (consume) these fibres, they produce beneficial substances which support a healthy gut lining and overall gut environment. You can find prebiotics in many different foods including onions, garlic, chicory and artichokes. These might be a little tricky to introduce to your little ones, however... Some can be easily hidden in pasta sauces, for example, but if you are struggling, you could consider a prebiotic or synbiotic supplement. Optibac Probiotics Kids Gummies, the newest addition to the Optibac Probiotics range, is a great choice as it contains both friendly probiotic bacteria and a prebiotic, in a delicious strawberry flavour gummy.
Aside from occasional treats, try to steer clear of sugar. Unfortunately, bad gut bugs love it as much as we do! We recommend swapping to wholegrain pasta or bread and snacking on homemade cereal bars to lower sugar consumption in quick, easy ways your little ones will hardly notice.

School
Like toddlers at nursery, children’s immune systems are challenged at school. Although it’s good to get a little bit of exposure, as discussed earlier, you also want your children to have the best defence system in place. We talk more about the role of friendly bacteria and immunity in the following blogs: All About The Microbiome and Probiotics: The 2020 way to support your immunity. Essentially, friendly bacteria help to modulate the immune system and train it to respond appropriately. A weakened immune system may not be as prepared to fight infections, meaning your child might take longer to recover from a school bug or illness.
Never fear, probiotics are here! A probiotic combination of three strains including Lactobacillus acidophilus Rosell 52 was trialled in children aged 3-7. The gold-standard study found the children who took a daily probiotic had a 25% reduction in risk of illness, compared to those who didn’t take a probiotic. There was a 40% risk reduction of missing school in the group taking probiotics compared to placebo10.
Another strain, Lactobacillus rhamnosus GG®, has been shown to reduce the risk and duration of upper respiratory infections in children29. In one study of 281 children, the length of time the children suffered with runny noses and sore throats was significantly shorter in those taking L. rhamnosus GG® for 3 months. Another study on L. rhamnosus GG® found the probiotic strain reduced the occurrence of respiratory illness in children attending day care centres30.
If you'd like to support your child's gut and immune health at school, try adding high-quality probiotic strains to their daily routine. L. rhamnosus GG mentioned in the trials above can be found in Optibac Probiotics Babies & Children.
We can see the research for probiotics and immune health is strong, but did you know that a child’s behaviour at school may be associated with their gut bacteria?
A recent study in January 2020, found that gut bacteria may be responsible for how a child behaves. They saw differences in the gut bacteria between poorly behaved children and those who were well-behaved. The researchers delved deeper into these differences and what may cause them. They looked at the relationship between the parents and child, parental stress levels and lifestyles on the microbiome. They found reduced levels of certain good bacteria were associated with poor behaviour. Plus, the parental stress levels and relationship quality between the parents and child were linked to changes in the microbiome11.
Other trials have shown the microbiome is associated with autism12. Health care professionals can find more information on probiotics and autism on our sister site, Probiotics Professionals.
Summary
There has been a lot of information in this blog! But the key takeaway is that childhood is one of the most important stages for the microbiome to develop. Imbalances between good and harmful bacteria may impact current and future health. There are, unfortunately, many factors which can cause these imbalances. However, high-quality probiotic supplements can step in and help to rebalance the microbiome and support overall health.
This article forms part 2 in our educational resource, ‘Early life microbiome series’, where we take you on a journey through the development and support of the microbiome from conception through to young adulthood. The other articles in this series are:
- All About The Microbiome
- Child Microbiome: Dr Kate's Guide - this explores the factors affecting the microbiome in childhood
- Probiotics for Pregnancy
- Baby Probiotics
- Probiotics for Kids
- Which probiotics are best for teenagers?
If you enjoyed this article, take a look at the following:
How to get kids to take probiotics
Start building your children's immunity now: Back to school health
Are cleaning products impacting your child's gut health?
Healthcare professionals can find more information on L. rhamnosus GG® and other strains listed in this article on our professionals site.
References
- Carroll F et al., “Factors influencing parents decision making when sending children with respiratory tract infections to nursery,” Journal of Public Health, vol. 38, pp. 281-288, 2016.
- Ownby et al., “Exposure to dogs and cats in the first year of life and risk of allergic sensitisation at 6 to 7 years of age.,” JAMA, vol. 119, no. 5, pp. 963-972, 2002.
- Cheema G et al., “Effect of prenatal dog exposure on eczema development in early and late childhood,” Annals of Asthma, Allergy and Immunology, vol. 119, no. 5, p. S14, 2017.
- Laynaert B et al., “Does living on a farm during childhood protect against asthma, allergic rhinitis and atopy in adulthood?,” AJRCCM, vol. 10, p. 164, 2001.
- Normand AC et al., “Airbourne cultivable microflora and microbial transfer in farm buildings and rural dwellings,” Occup. Environ. Med, vol. 68, pp. 849-855, 2011.
- Christian LM et al., “Gut microbiome composition is associated with temperament during early childhood,” Brain, Behav, Immun, vol. 45 , pp. 118-127, 2015.
- Aatsinki A et al., “Gut microbiota composition is associated with temperament traits in infants,” Brain, Behaviour and Immunity, pp. 80: 849-858, 2019.
- Nicolini G et al., “Combating the rise of antibiotic resistance in children,” Minerva Pediatri, vol. 66, no. 1, pp. 31-9, 2014.
- Schwartz et al., “Antibiotic use and childhood body mass index trajectory,” International Journal of Obesity , vol. 40, p. 615–621, 2015.
- Cazzola, “Efficacy of a synbiotic supplementation in the prevention of common winter diseases in children: a randomised, double blind, placebo-controlled pilot study,” Therapeutic advances in respiratory disease, vol. 4, no. (5), pp. 271-8, 2010.
- Flannery J et al., “Gut feelings begin in childhood: the gut metagenome correlates with early environment, caregiving and behaviour.,” Am. J. Micro, vol. 11, no. 1, pp. e02780-19, 2020.
- Vuong et al., “Emerging Roles for the Gut Microbiome in Autism Spectrum Disorder,” Biological Psychiatry, vol. 81, no. 5, pp. 411-423, 2017.
- Sheo Y et al., “Stunded microbiota and opportunistic pathogen colonisation in caesarean section birth,” Nature, pp. 574 (7776): 1-5, 2019.
- Betran A et al., “The increasing trend in Caesarean section rates: global, regional and national estimates,” PLoS ONE, vol. 11, pp. 11- e0148343, 2016.
- Alarming global rise in caesarean births, figures show, 368; doi10.1136/bmj.k4319: BMJ, 2018.
- Tamburini S et al., “The microbiome in early life: implications for health outcomes,” Nature Medicine , pp. 22 (7): 713-722, 2016.
- Sevelsted A et al., “Ceasarean section and chronic immune disorders,” Pediatrics, vol. 135, pp. 92-98, 2015.
- Wu T et al., “Infant and adult inhalation exposure to resuspended biological particulate matter,” Environ. Sci. Technol, vol. 52, no. 1, pp. 237-247, 2018.
- S Lynch et al., “Effects of early-life exposure to allergens and bacteria on recurrent wheeze and atopy in urban children,” Journal of Allergy and Clinical Immunology, p. DOI: 10.1016/j.jaci.2014.04.018, 2014.
- Hesselmar B et al., “Pacifier cleaning practises and risk of allergy development,” Pediatrics, vol. 131, pp. e1829-e1837, 2013.
- Nicolini G et al., “Combating the rise of antibiotic resistance in children,” Minerva Pediatr, vol. 66, no. 1, pp. 31-9, 2014.
- Risnes KR et al., “Antibiotic exposure by 6 months and asthma and allergy at 6 years: findings in a cohort of 1401 US children,” Am. J. Epidemiol, vol. 173, pp. 310-318, 2011.
- Hoskin-Parr L et al., “Antibiotic exposure in the first two years of life and development of asthma and allergic diseases by 7.5 yr: A dose dependent relationship,” Pediatric allergy and immunology, pp. 24 (8): 762-771, 2013.
- Saari A et al., “Antibiotic exposure in infancy and risk of being overweight in the first 24 months of life,” Pediatrics, pp. 135 (4): 617-626, 2015.
- Droste JH et al., “Does the use of antibiotics in early childhood increase the risk of asthma and allergic disease,” Clin Exp Allergy, vol. 30, no. 11, pp. 1574-53, 2000.
- Schwartz BS et al., “Antibiotic use and childhood body mass index trajectory,” Int J. Obes (Lond), vol. 40, pp. 615-621, 2016.
- Kronman MP et al., “Antibiotic exposure and IBD development amoung children: a population based cohort study,” Pediatrics, vol. 130, pp. 794-803, 2012.
- Messaoudi M et al., “Beneficial psychological effects of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers,” Gut Microbes, vol. 2, no. 4, pp. 256-61, 2010.
- Hojsak et al., (2010) Lactobacillus GG in the prevention of gastrointestinal and respiratory tract infections in children who attend day care centers: a randomized, double-blind, placebo-controlled trial. Clinical Nutrition, 29(3): 312-6.
- Kumpu M et al., (2012) Milk containing probiotic Lactobacillus rhamnosus GG and respiratory illness in children: a randomized, double-blind, placebo-controlled trial. European Journal of Clinical Nutrition, 66(9):1020-3.
Popular Articles
View all Children's Health articles-
Children's Health25 Oct 2023
-
Children's Health12 Oct 2023