Study: 'Lacidofil' Formula & Antibiotics
The results of a new Canadian study just published in the British Journal of Nutrition, have confirmed that probiotics can help with the management of antibiotic-associated diarrhoea (AAD).
Antibiotics can be a life-saving medication and, since their accidental discovery by Professor Alexander Fleming on September 3rd, 1928, they have become a widely-used tool in every doctor’s arsenal of drugs. Once begun, it’s very important to complete the course of this medication, but many people experience unpleasant side effects and discontinue their antibiotic treatment.

One very common side effect is antibiotic-associated diarrhoea (AAD), and researchers have been looking for a viable and safe solution to this problem for some time. It occurs in around 5-30% of patients either during antibiotic therapy, or even up to two months after the treatment has been completed. The level of severity can vary, ranging from mild diarrhoea to severe pseudomembranous colitis which can be life-threatening1. Many probiotics can be ineffective during antibiotic courses, as the indiscriminate action of the drugs kills beneficial bacteria along with pathogenic species, one reason why many people choose to supplement with probiotics post-antibiotic therapy.
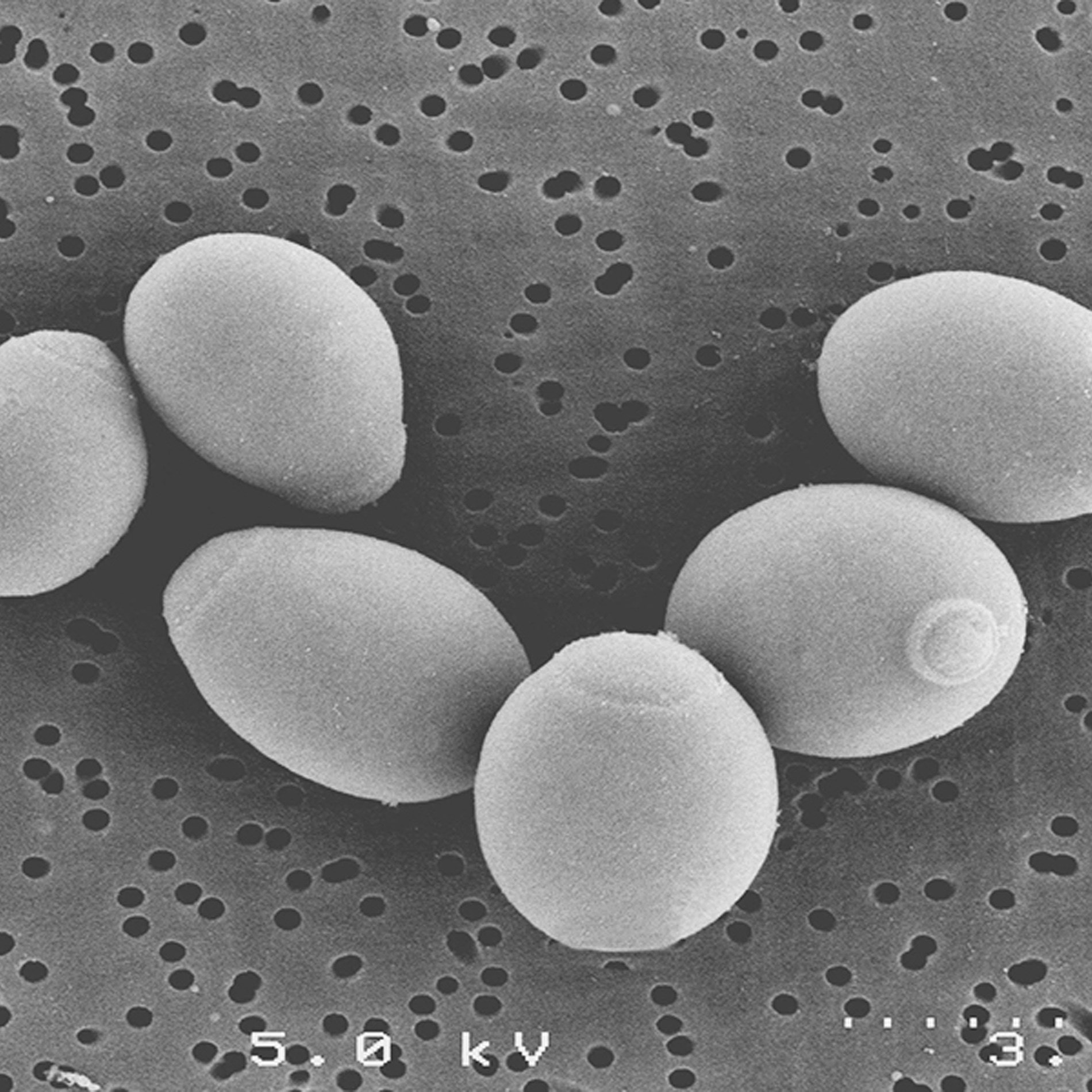
The probiotic used in the clinical trial was a combination of two Lactobacillus species, (Lactobacillus rhamnosus Rosell-11 and Lactobacillus helveticus Rosell-52) known collectively as ‘Lacidofil’. Lacidofil is an extremely well-researched formula that is supported by 26 clinical trials that used a total of 1,700 children and adults, giving it drug status in some countries.
In this latest ‘gold standard’ randomised double-blind, placebo-controlled clinical trial using 146 healthy adults, Lacidofil was shown to reduce the incidence and duration of AAD by around 24 hours2. The subjects were all given a broad spectrum antibiotic treatment (am***cillin-clavulanic acid) for one week. Alongside this medication, and for one week afterwards, some of the participants were given the Lacidofil probiotic formula, whilst others were given a placebo. The results indicated that those given the probiotic suffered AAD symptoms for a significantly shorter period of time than those in the placebo group; this is the first study to use healthy adults as subjects and show a clinical benefit.
Lacidofil probiotic viable alongside antibiotics?
Stool samples collected throughout the trial, and the subjects were monitored for nine weeks after the antibiotic therapy had finished to ascertain the viability of the probiotic strains in Lacidofil, Lactobacillus rhamnosus Rosell-11 and Lactobacillus helveticus Rosell-52. Testing of the fecal samples suggested that both strains survived transit through the intestinal tract and, even more importantly, were able to survive even when administered at the same time as the broad-spectrum antibiotic treatment. This finding appears to dispel the commonly-held belief that you can’t take probiotics alongside antibiotics – it’s all about using the correct strains. Head over to the Learning Lab to see our latest Probiotic ‘Myth-buster’: The Antibiotics Myth to find out more about taking probiotics with antibiotics.
Health Professionals can also head to the Probiotics Database to learn more about Lactobacillus rhamnosus Rosell-11 and Lactobacillus helveticus Rosell-52
The trial builds on the results from other AAD/Lacidofil studies, three that were conducted using adults and seven using child subjects. The researchers were very excited by these results, and had this to say about their findings:
“Decreasing the number of days of diarrhoea after antibiotic treatment has clinical relevance, as it may reduce complications related to AAD. This is particularly important among patients who are more susceptible to severe AAD, as well as in attenuating the symptoms of AAD in individuals with a healthy digestive system receiving antibiotics for infections outside the gut.”
Antibiotics have saved many lives, and this study demonstrates that it’s not about looking for an alternative, but to help the drugs to work more efficiently and be better tolerated. Head to the Learning Lab to read our blog ‘Antibiotics v probiotics? You’re asking the wrong question’.
For related articles and information pages, click on the following links:
Blog: Can probiotics help prevent antibiotic resistance?
Media: Optibac Probiotics mentioned in new book ‘Antibiotics: Are they curing or killing us?’
References
- Frédéric Barbut (2002), Managing antibiotic associated diarrhoea, BMJ, 2002 Jun 8; 324(7350): 1345–1346.
- Evans, M. et al (2016), Effectiveness of Lactobacillus helveticus and Lactobacillus rhamnosus for the management of antibiotic-associated diarrhoea in healthy adults: a randomised, double-blind, placebo-controlled trial, British Journal of Nutrition, 2016 Jul;116(1):94-103. doi: 10.1017/S0007114516001665. Epub 2016 May 12.
Popular Articles
View all General Health articles-
General Health13 Feb 2024