Probiotics for digestive health
The function of our digestive system is to break foods down into small particles for our cells to use for energy. Did you know that bacteria play a huge part in our digestion, helping us to produce vitamins and digest certain food groups?
In this article, we will answer the question ‘Do probiotics help your digestive system?’ And ‘Is there a role for probiotics in the support of digestion and bloating?
We will also look at:
- What do probiotics do for digestion?
- Are probiotics good for digestion?
- Best probiotics for digestive health
- What are the signs you need probiotics?
- Are probiotics good for an upset stomach?
What do probiotics do for digestion?
We know that optimal digestion is critical to our long-term health, so let’s take a closer look at how our digestion works and the benefits of probiotics for the stomach. When all nutrients have been absorbed, water, bacteria and fibre pass through to the large intestine. Around two-thirds of our stool is composed of water and undigested fibre and food products. The other third is composed of living and dead bacteria. In fact, the large intestine contains trillions of bacteria, also known as probiotics.
One way that bacteria directly facilitate digestion is that certain bacteria can make lactase which is needed in order to break down milk proteins. The most fascinating role of bacteria in supporting human digestion is their ability to ferment dietary fibre, to produce something called Short Chain Fatty Acids (SCFA’S), such as; butyric acid, propionic acid and acetic acid. Which are the main fuel source for the cells of our colon. These short-chain fatty acids strengthen the integrity of our colon to enable proper digestion of fats, proteins, and starches, whilst at the same time providing a physical barrier to keep out any foreign substances.
This is why it is so vital that our diet consists of plenty of prebiotics, from fruits, vegetables, beans, nuts and seeds, as without adequate fibre, we essentially starve our colonic cells and weaken the gut lining1. Interestingly, as humans, we cannot fully digest the fibre in plant foods. Instead, undigested fibre travels down to our colons where our bacteria use this fibre as a food and energy source to grow and thrive which directly benefits our health and well-being, not to mention digestion.

Are probiotics good for digestion?
As discussed above, probiotics play a vital role in digestion and work synergistically with us. But how exactly are probiotics beneficial for our digestion? Well, bacteria help to lower the pH of the colon 2, making the conditions of our gut less favourable to pathogens. Probiotics also speed up peristalsis , which is the muscle movement which continuously moves food through our digestive system. This is because they can help to rebalance the gut microbiome and an imbalance in gut bacteria is thought to slow down transit time. Conversely, peristalsis can also be sped up, if our immune system is alerted that we have ingested something harmful, this is to remove it from our digestive system as soon as possible before it causes us any harm.
Finally, I mentioned that the fibre from our diet is what feeds our gut bacteria, producing short-chain fatty acids. It is these acids that help us produce and manufacture lots of vitamins such as B Vitamins, Vitamin A and K. It is also believed that our gut bacteria play a role in Vitamin D absorption3. So, to answer the question, are probiotics good for digestion, the answer is yes as they play such a vital role in this complex bodily process. Starting with digestive enzymes, which are produced in the pancreas and help us digest fats, carbohydrates and proteins. Meanwhile, in the large intestine, undigested fibre is fermented by our gut bacteria, producing short-chain fatty acids and vitamins.4
For more information on probiotics for digestion and digestive enzymes, please take a look at the following page which discusses digestive enzymes in great depth.
Best probiotics for digestive health
The best probiotic for digestive health will depend on your specific needs. Which is why it’s important to select the right strains for you. We also want to encourage diversity within our gut microbiome. Having plentiful levels of beneficial live bacteria take up space in the gut, meaning there is less space for unfavourable pathogens or bacteria to grow and become established.
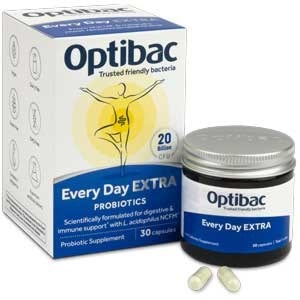
The two genus groups that make up the majority of a healthy human gut are lactobacillus and Bifidobacterium which are found predominately in the colon. It is important when looking to address digestive issues to find the right strain for you. For example, Lactobacillus acidophilus NCFM®, is the most clinically researched strain of acidophilus and has been shown to reduce abdominal pain, so can be extremely helpful for those who experience IBS related to abdominal cramping, spasms and pain. On the other hand, for those who experience constipation, the strain Bifidobacterium lactis BB-12® is the most clinically trialled strain for constipation. Healthcare professionals can read more about Lactobacillus acidophilus NCFM® and Bifidobacterium lactis BI-07® on the probiotics database.
To help you find the right probiotic for you, please read our article: Best probiotics for gut health.
What are the signs you need probiotics?
If you experience any of the following signs and symptoms it may suggest that your digestive system could benefit from a probiotic supplement which promotes good gut health.
- Bloating
- Gas
- Diarrhoea
- Constipation
- IBS
- Abdominal cramps
- Indigestion5
Other less-known indicators may be:
- Poor sleep6
- Joint pain 7
- Food intolerances8
- Autoimmunity9
- Frequent UTIs10
- Low mood11

Are probiotics good for an upset stomach?
A question we often get asked is, are probiotics good for an upset stomach? The answer is yes. As probiotics can help restore the normal balance following stomach upset, which may be caused by illness, certain treatments or medication. One of the reasons that probiotics may be helpful is because following stomach upset, such as diarrhoea, often the number and diversity of our live bacteria are greatly reduced. If not restored, this may result in dysbiosis (an imbalance in our gut bacteria), which is thought to be responsible for many long-term digestive issues. Therefore, a probiotic or the regular consumption of foods which contain live bacteria can help to rebalance our gut microbiome.
This is important as our gut bacteria act as gatekeepers to ward off any harmful pathogens. The more beneficial bacteria we house the less space there is for opportunistic pathogens to take hold, so probiotics for the stomach can be extremely helpful. This is also why we recommend taking a probiotic alongside antibiotic medication or when travelling to foreign countries to reduce the risk of an upset stomach. Since live bacteria help to reduce dysbiosis and modulate your immune system they are a great long-term daily practice to keep your gut in tip-top condition. So why not try probiotic supplements for digestive health? As this is a great example of when you should take probiotics for digestion.
Summary
We have covered a lot in this article, so here is a short summary of the main points:
- Bacteria play a key role in our digestion.
- You may benefit from taking a probiotic if you have; bloating, constipation, diarrhoea or stomach pain.
- The best probiotic for digestive health will depend on your specific needs.
- Probiotics may help an upset stomach due to their ability to out crowd invading bacteria or pathogens.
Hopefully, this article has helped you understand how probiotics support our digestive health. If you are interested in reading more about digestion, please check out the following articles:
Probiotics for Bloating
Benefits of Probiotics
Best Probiotics for Gut Health
References
- Petersson J. (2011). Importance and regulation of the colonic mucus barrier in a mouse model of colitis. Am J Physiol Gastrointest Liver Physiol.. 0(0).
- Cremer J. (2017). Effect of water flow and chemical environment on microbiota growth and composition in the human colon. Proc Natl Acad Sci USA. 0(0), p.0.
- Jones, M. (2013). Oral supplementation with probiotic L. reuteri NCIMB 30242 increases mean circulating 25-hydroxyvitamin D. :a post hoc analysis of a randomized controlled trial. J. Clin. Endocrinol. Metab.. 0(0), p.0. [Online].
- Xu J. (2003). Honour thy synbionts. Proc. Natl. Acad. Sci. USA.. 0(0), p.0.
- Kassinen A. (2007). The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology. 0(0), pp.24-33.
- Eriksson EM,. (2015). Aspects of the non-pharmacological treatment of irritable bowel syndrome. World J Gastroenterol. 0(0), p.0.
- Furst D.E. (2010). The risk of infections with biologic therapies for rheumatoid arthritis. Semin. Arthritis Rheum. 0(0), p.327–346.
- Molloy J. (2013). The potential link between gut microbiota and IgE-mediated food allergy in early life. Int. J. Environ. Res. Public Health. 0(0), p.7235–7256.
- Brown K. (2012). Diet-induced dysbiosis of the intestinal microbiota and the effects on immunity and disease. Nutrients. 0(0), p.0.
- Lemberger U. (2021). The microbiome in urinary tract infections in children—An update. Curr. Opin. Urol. 0(0), p.147–154.
- Mohajeri MH. (2018). 11. Relationship between the gut microbiome and brain function. Nutr Rev. 0(0), pp.481-496.